Diagnosis of Ankylosing Spondylitis
Diagnosing ankylosing spondylitis can be challenging because its symptoms often mimic general back pain. Diagnosis of Ankylosing Spondylitis usually combines clinical signs, imaging, and blood tests.
Step 1: Medical History and Physical Examination
Your doctor will assess:
- Duration and pattern of back pain (especially pain that improves with activity)
- Morning stiffness and its duration
- History of eye inflammation (uveitis), bowel symptoms, or joint pain
- Family history of AS or related conditions
Physical tests may include:
- Spinal flexibility measurements
- Chest expansion testing
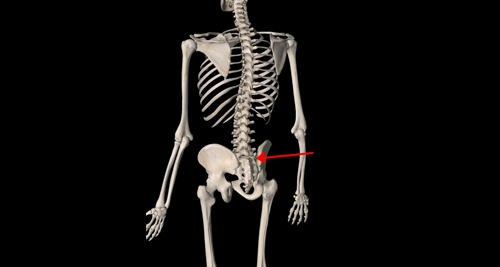
- Tenderness over sacroiliac joints
Step 2: Imaging
- X-rays of the lower spine and pelvis may show sacroiliac joint inflammation or spinal fusion
- In early disease, X-rays may appear normal
- MRI is more sensitive and can detect early inflammation before permanent damage occurs
Step 3: Laboratory Tests
- HLA-B27 testing – Presence supports diagnosis but is not definitive
- CRP and ESR – Inflammatory markers may be elevated but can be normal in some cases
- Rheumatoid factor (RF) – Negative in AS (helps rule out rheumatoid arthritis)
Differential During Diagnosis of Ankylosing Spondylitis
AS must be distinguished from:
- Mechanical low back pain
- Degenerative disc disease
- Fibromyalgia
- Psoriatic arthritis
In South Africa, AS may be underdiagnosed, especially in rural areas with limited access to rheumatologists and MRI. Early referral improves outcomes significantly.
👉 [Next: Treatment for Ankylosing Spondylitis]
Causes and Risk Factors of Ankylosing Spondylitis