Diagnosis of Bursitis
Diagnosis of bursitis involves evaluating a person’s symptoms, physical condition, and sometimes using imaging or lab tests to rule out other conditions. A proper diagnosis of bursitis allows for effective treatment and helps prevent complications like chronic pain or joint damage.
Doctors begin by taking a full medical history, asking about the onset, location, duration, and triggers of the pain. They also consider occupational or recreational activities that may contribute to joint overuse.
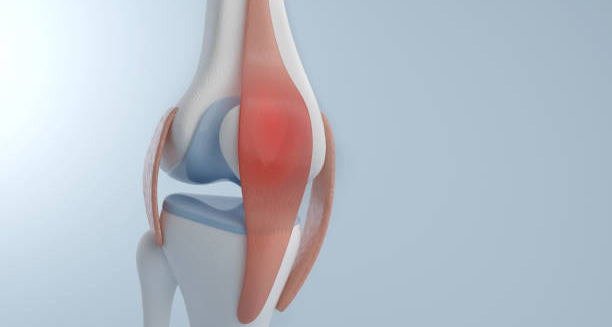
During the physical exam, the doctor will inspect the affected joint for swelling, redness, warmth, and tenderness. They may also check your range of motion and identify specific movements or postures that trigger discomfort.
In most straightforward cases, diagnosis is clinical and no further testing is needed. However, when symptoms are severe, persistent, or involve signs of infection, additional tools may be used:
- X-rays can help rule out arthritis, bone spurs, or fractures but don’t show bursae directly.
- Ultrasound provides detailed images of soft tissues and is excellent for detecting fluid in the bursa.
- MRI is occasionally used to evaluate deeper or complex cases where multiple joint issues are suspected.
- Aspiration of bursal fluid may be done if infection is suspected. A needle is used to withdraw fluid, which is then tested for bacteria, white blood cells, or uric acid crystals.
Diagnosis of Bursitis
Blood tests may also be ordered to check for infection markers, autoimmune diseases, or gout, particularly in recurrent or unexplained cases of bursitis.
In chronic cases or where structural abnormalities are involved, referral to a rheumatologist, orthopaedic specialist, or physiotherapist may be needed for further evaluation.
A correct diagnosis of bursitis ensures that treatment is tailored appropriately — whether rest and ice will suffice or if medical procedures, antibiotics, or rehabilitation are required.
[Next: Treatment of Bursitis →]