Causes of Frozen Shoulder
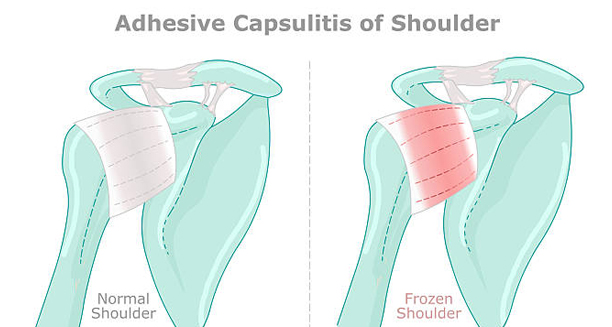
The causes of frozen shoulder involve inflammation and thickening of the shoulder joint capsule, which restricts movement. Frozen shoulder can develop without an obvious reason (primary) or as a result of injury or medical conditions (secondary).
Primary Frozen Shoulder
In many cases, frozen shoulder occurs without any clear cause. This is known as idiopathic or primary frozen shoulder. It’s believed that:
Inflammation causes the joint capsule to thicken and contract
Adhesions (bands of scar-like tissue) form inside the joint
Synovial fluid (which lubricates the joint) may be reduced
Why this happens in otherwise healthy people remains unclear, but certain risk factors increase susceptibility.
Secondary Frozen Shoulder
This type develops following another condition or event that affects the shoulder:
Shoulder injury or surgery – dislocations, fractures, or operations can lead to immobilisation
Rotator cuff problems – such as tears or tendonitis
Stroke – paralysis or reduced use of the arm may trigger stiffness
Heart surgery – some people develop frozen shoulder after open-heart procedures
Any situation that limits arm movement for a prolonged period can increase the risk of adhesive capsulitis.
Medical Risk Factors
Certain health conditions are strongly linked to frozen shoulder:
Diabetes – one of the most significant risk factors; affects 10–20% of diabetics
Thyroid disorders – both overactive and underactive thyroid conditions
Parkinson’s disease – due to muscle stiffness and reduced mobility
Cardiovascular disease
People with autoimmune disorders or metabolic syndrome may also have an increased risk.
Age and Gender
Most common between ages 40 and 60
Women are affected more than men
The non-dominant shoulder is often involved, though either side can be affected
Causes of Frozen Shoulder
Understanding the causes of frozen shoulder is essential for prevention, especially in people with diabetes or those recovering from upper body injuries or surgery.