Diagnosis of Glomerulonephritis
The diagnosis of glomerulonephritis is based on a combination of clinical history, physical examination, laboratory tests, and sometimes a kidney biopsy. Because glomerulonephritis can present subtly or mimic other conditions, accurate diagnosis is essential to prevent mismanagement and to tailor treatment effectively.
Early diagnosis offers the best chance of preserving kidney function. With advances in diagnostic technology, doctors can now detect even small changes in kidney structure and function long before symptoms appear.
Medical History and Clinical Examination
The diagnostic process begins with a comprehensive medical history, where the doctor explores:
Recent infections (e.g., strep throat, skin infections)
Autoimmune diseases (e.g., lupus, vasculitis)
Family history of kidney disease
Medications, including NSAIDs or antibiotics
Exposure to toxins, illicit drugs, or heavy metals
A physical exam checks for:
Oedema in the legs, face, or abdomen
Elevated blood pressure
Signs of fluid overload, such as lung crackles
Skin rashes or joint inflammation (suggestive of systemic autoimmune disease)
Urinalysis: The Cornerstone of Diagnosis
Urine tests are often the first clue in identifying glomerulonephritis. Important findings include:
Proteinuria – high levels of protein in the urine
Haematuria – microscopic or visible blood
Casts – tube-shaped particles made of proteins or cells, indicating kidney inflammation
White or red blood cells – signalling infection or inflammation
Dipstick urinalysis is useful for screening, while 24-hour urine collection quantifies protein loss.
Blood Tests
Several blood tests support the diagnosis and help identify underlying causes:
1. Kidney Function Tests
Creatinine and urea: Elevated levels suggest impaired filtration
Estimated glomerular filtration rate (eGFR): Indicates overall kidney function
2. Electrolyte and Metabolic Panels
Assess sodium, potassium, calcium, phosphate
Check acid-base balance
3. Complete Blood Count (CBC)
May show anaemia (from chronic kidney disease)
Elevated white cells in infection or inflammation
4. Autoimmune Markers
ANA (antinuclear antibodies) for lupus
ANCA for vasculitis
Anti-GBM antibodies for Goodpasture syndrome
Complement levels (C3, C4) – often low in post-infectious or lupus nephritis
5. Viral Serologies
Tests for hepatitis B, hepatitis C, and HIV
Essential in cases of secondary glomerulonephritis
Imaging Studies
While not diagnostic on their own, imaging helps assess kidney structure and rule out other issues.
1. Renal Ultrasound
Non-invasive and widely used
Detects kidney size, cysts, or obstruction
Helps assess chronicity (e.g. shrunken kidneys in longstanding disease)
2. CT or MRI
Rarely required but useful if complications are suspected
Kidney Biopsy: The Definitive Test
When the cause of glomerulonephritis is uncertain or the disease appears severe, a kidney biopsy may be necessary. This involves:
Using a needle to take a small sample of kidney tissue
Examining it under a microscope for signs of inflammation, scarring, or immune deposits
A biopsy can:
Confirm the specific subtype (e.g. IgA nephropathy, membranous nephropathy)
Guide treatment decisions (e.g. steroid use, immunosuppressants)
Help determine prognosis
Biopsies are typically safe and performed under local anaesthesia with ultrasound guidance.
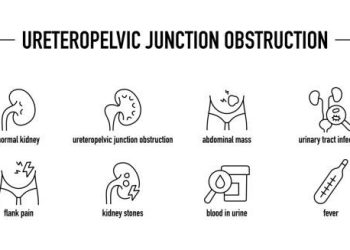
Differential Diagnosis
Several other conditions can mimic glomerulonephritis. A careful diagnostic process distinguishes it from:
Urinary tract infections
Interstitial nephritis
Nephrotic syndrome of other causes
Polycystic kidney disease
Diabetic nephropathy
Proper differentiation ensures the correct therapy and prevents further damage.
Diagnostic Summary Table
| Test | Purpose |
| Urinalysis | Detects blood, protein, and casts |
| Blood tests | Assess kidney function and inflammation |
| Autoimmune markers | Identify systemic causes |
| Imaging | Visualise kidney structure |
| Kidney biopsy | Definitive diagnosis and disease classification |
When to Refer to a Specialist
Patients with signs of glomerulonephritis should be referred to a nephrologist if they:
Have significant proteinuria or haematuria
Show signs of rapid kidney deterioration
Have resistant hypertension
Need a biopsy or immunosuppressive therapy
Early referral improves outcomes by allowing for targeted treatment before irreversible damage occurs.
Conclusion | Diagnosis of Glomerulonephritis
The diagnosis of glomerulonephritis involves a step-by-step evaluation using urine and blood tests, imaging, and sometimes biopsy. Accurate diagnosis is critical not only to confirm the condition but also to determine the underlying cause and appropriate treatment. With early detection and ongoing monitoring, patients can avoid complications and preserve their kidney health long term.