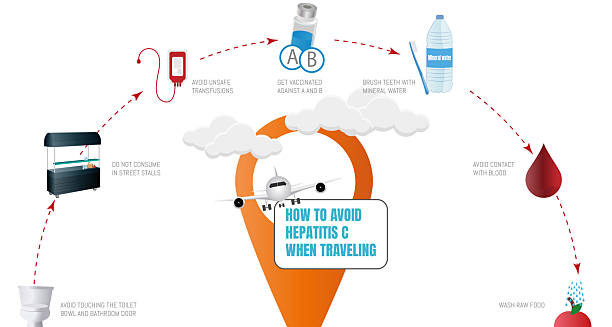
The prevention of hepatitis C is one of the most powerful tools in combating the global burden of liver disease, particularly since there is no vaccine for the hepatitis C virus (HCV).
Unlike hepatitis A or B, hepatitis C cannot be prevented by a vaccine. Instead, stopping the spread depends on avoiding blood exposure, raising awareness, and following strict safety practices. Even though treatment can cure hepatitis C, prevention is still the most effective way to protect people, especially in high-risk and underserved communities.
Stopping Blood-to-Blood Contact
The main way hepatitis C spreads is through direct contact with infected blood. To prevent this:
- Do not share needles, syringes, or drug equipment
- Avoid sharing razors, toothbrushes, or nail clippers
- Always use clean tools when treating wounds
People who inject or use drugs through the nose should receive support, education, and access to harm reduction services to lower their infection risk.
Hepatitis A and Safer Drug Use
People who inject drugs account for many new hepatitis C cases. Safe practices include:
- Needle and syringe programs (NSPs) that offer clean supplies
- Supervised drug-use centers that reduce unsafe injecting
- Opioid treatments like methadone to lower the need for injecting
- Fast testing and early treatment to reduce spread in the community
These steps have been proven to reduce new infections. They are supported by health groups such as the World Health Organization.
Safe Medical and Dental Care
Clean and careful practices in clinics and hospitals can stop hepatitis C from spreading. Healthcare workers should:
- Sterilize tools after each use
- Use new gloves and needles for every patient
- Dispose of sharp items in proper containers
- Screen all donated blood and organs
Unsafe medical care is still a problem in some countries. Better training and cleaner equipment can prevent many infections.
Safer Tattooing and Piercing
Getting a tattoo or piercing can be risky if done in an unsafe setting. To reduce that risk:
- Choose licensed shops that follow hygiene rules
- Make sure they use fresh needles and ink each time
- Avoid tattooing in informal places like prisons or homes
Professionals should also get training on preventing infections such as hepatitis C and Hepatitis A.
Keeping Healthcare Workers Safe
Doctors, nurses, and emergency workers face risks from sharp tools or blood contact. They can stay safe by:
- Wearing gloves, masks, and gowns
- Using needles with safety features
- Following clear post-exposure procedures
- Learning how to handle blood safely
A single needlestick injury has a small risk of spreading hepatitis C, but it’s easy to avoid with the right gear and training.
Reducing the Risk of Sexual Transmission
While sexual transmission of hepatitis C is less common, it still happens. The risk is higher in:
- Men who have sex with men (MSM), especially those with HIV
- People who have multiple partners or sexually transmitted infections (STIs)
Using condoms and discussing safety with partners helps lower the risk. If one person has hepatitis C, the other should get tested and learn how to stay protected.
Preventing Mother-to-Child Transmission
A small number of babies—about 5 to 6 percent—born to mothers with hepatitis C may become infected. To reduce this:
- Screen pregnant women, especially those with risk factors
- Track the virus during pregnancy
- Test the baby after birth
While current treatments are not approved during pregnancy, women can be treated before getting pregnant or between pregnancies to protect future children.
Education and Stigma Reduction
Many people don’t understand how hepatitis C spreads, which leads to fear and missed diagnoses. Public education should:
- Explain that hepatitis C does not spread through hugging, kissing, or shared meals
- Encourage testing for people with tattoos, time in prison, or past transfusions
- Reduce shame that keeps people from seeking help
- Promote the fact that hepatitis C is curable
Social media, community outreach, and school programs can all help change public opinion and encourage safe choices.
Screening and Connecting People to Care
Many countries now recommend hepatitis C testing for:
- Adults aged 18 to 79
- All pregnant women
- People with risky behaviors or jobs
Testing finds people early and allows fast treatment. This protects their health and also prevents them from infecting others. Connecting people to care quickly helps stop the spread. Once cured, a person can no longer transmit hepatitis C, making treatment an effective form of prevention.
Global Goals and the Role of Hepatitis A
The World Health Organization hopes to eliminate hepatitis C as a major health threat by 2030. Their goals include:
- A 90% drop in new cases
- A 65% drop in deaths
To reach these goals, we must:
- Expand harm reduction programs
- Make treatment more affordable
- Increase testing and education
- Improve healthcare safety worldwide
Vaccinating against Hepatitis A is also vital, especially for people with liver disease. Getting both infections can cause liver failure, so preventing Hepatitis A protects people already at risk.
In Summary
Preventing hepatitis C depends on smart choices, clean environments, and early care. Even without a vaccine, the virus is fully preventable. Reducing blood exposure, testing at-risk groups, and linking people to care can stop new cases. These efforts not only protect individuals but also bring the world closer to ending hepatitis C for good. Small steps like Hepatitis A vaccination and safe injection practices make a big difference.