The symptoms of hereditary haemorrhagic telangiectasia (HHT) are highly variable in presentation, severity, and age of onset.
This rare blood vessel disorder causes weak connections between arteries and veins. These can bleed or burst easily. Some people have only mild symptoms for years, while others face serious problems. That’s why it’s so important to understand all possible signs of this condition. Early detection can lead to better treatment and fewer risks.
Nosebleeds (Epistaxis)
Nosebleeds are the most common and often first symptom of HHT. Around 90% of people with this condition get them. They happen because of tiny, weak blood vessels inside the nose. These break easily from dry air, small bumps, or even during sleep.
What to expect:
- How often: Some have rare nosebleeds. Others get them daily.
- How long: They might last a few seconds or go on for minutes.
- How bad: Light spotting is common, but some lose a lot of blood and get anaemia.
- When it starts: Usually in childhood or teenage years, and it can worsen with age.
For many, frequent nosebleeds affect their daily lives. They may feel embarrassed or need medical care if it becomes too much.
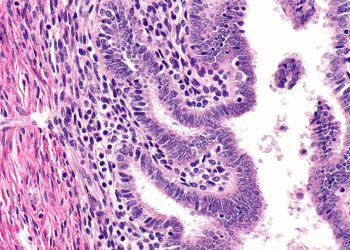
Skin and Mouth Lesions (Telangiectases)
Small red or purple spots can show up on the skin or inside the mouth. These are clusters of weak blood vessels close to the surface.
Where they appear:
- Face (especially around the nose and lips)
- Hands and fingers
- Tongue, gums, and cheeks
- Nail beds
These spots usually don’t hurt. They may bleed if scratched, but most of the time, people worry more about how they look. Their presence also helps doctors confirm the diagnosis.
Gastrointestinal Bleeding
As people with HHT get older, they may develop weak blood vessels in the stomach or intestines. These can break and cause slow, hidden bleeding.
Common signs:
- Black or tar-like stool
- Tiredness from blood loss
- Iron-deficiency anaemia
Visible bleeding is rare, but the damage builds up over time. It’s more common in people over 40 and in HHT type 2. Often, doctors spot it during blood tests.
Lung AVMs (Pulmonary Arteriovenous Malformations)
In about half of HHT patients, abnormal vessels form in the lungs. These let blood skip past the lungs’ oxygen exchange system, causing problems.
Symptoms include:
- Shortness of breath, especially when active
- Feeling tired easily
- Blue lips or fingers (due to low oxygen)
- Clubbed fingers (in severe cases)
- Migraines or blurred vision
The biggest danger is a paradoxical embolism. This is when clots or germs go through the lungs and reach the brain, leading to stroke or brain infection. Treatment often includes embolisation, a simple procedure that blocks the faulty vessels.
Brain AVMs and Serious Complications
Brain AVMs are less common but very dangerous. They can cause strokes, seizures, or nerve damage. They might be present at birth and not show up until a crisis.
Warning signs:
- Headaches or seizures
- Weakness or numbness
- Balance problems
- Sudden collapse
These are more likely in kids or young adults with the ENG gene (HHT type 1). Doctors usually recommend MRI scans, especially in families with known cases.
Hepatic AVMs (Liver Involvement)
AVMs in the liver might not show signs at first. Over time, they can cause serious issues, especially in HHT type 2.
What to look for:
- Stomach pain or a full feeling
- Enlarged liver
- Yellow skin (jaundice)
- Heart problems from too much blood flow
Doctors often find these during scans for other reasons. Severe cases may need a liver transplant, but most can be managed with careful care.
Spinal AVMs and Rare Effects
Spinal AVMs are uncommon but can cause big problems, especially in children.
Possible symptoms:
- Back pain
- Numbness or tingling
- Trouble walking or using legs
- Bladder or bowel issues
If these signs appear, doctors use spine MRIs to check for problems.
Tiredness and Anaemia
Ongoing bleeding—whether from the nose or stomach—can lead to iron-deficiency anaemia. This makes people feel weak and out of breath.
Symptoms include:
- Tiredness
- Dizziness
- Pale skin
- Fast heartbeat
Iron pills or transfusions can help. But managing the bleeding is the best way to feel better over time.
Variation in Symptoms Between Individuals
Not everyone with HHT has the same experience. Some get only light nosebleeds. Others may need regular hospital care.
Things that affect how bad symptoms are:
- The type of gene change (ENG, ACVRL1, or SMAD4)
- Age – problems often get worse over time
- Gender – women may have more liver issues
- Lifestyle – alcohol, smoking, or pregnancy can make symptoms worse
Hepatitis A and HHT Risk Comparison
While Hepatitis A mainly affects the liver and spreads through food or water, HHT impacts blood vessels throughout the body. Yet both conditions can lead to serious health issues if untreated. It’s important to manage both early and effectively. In patients with HHT, liver health is already at risk, so avoiding infections like Hepatitis A is also important.
In Summary
The symptoms of hereditary haemorrhagic telangiectasia range from mild bleeding to life-threatening AVMs in key organs. Nosebleeds are usually the first sign, but issues can arise in the lungs, brain, liver, and more. Early diagnosis and ongoing care are key to a better life. Just like with Hepatitis A, tracking symptoms and acting early helps avoid long-term damage.
[Next: Treatment of Hereditary Haemorrhagic Telangiectasia →]