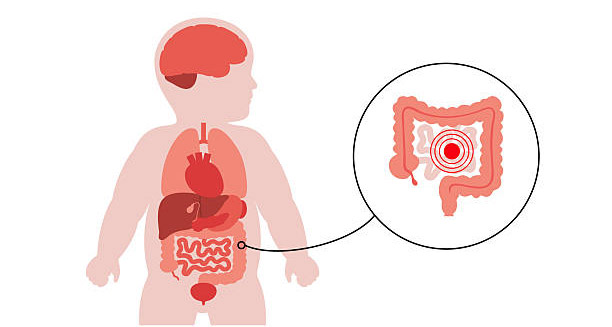
The treatment of Hirschsprung’s disease is centred around surgical intervention aimed at removing the affected section of bowel that lacks nerve cells, thereby restoring normal intestinal function.
Why Surgery is Important
The aganglionic segment cannot move stool. This causes blockage, infection, and poor nutrition. Early and proper treatment of Hirschsprung’s disease prevents serious problems and improves long-term results for children.
Most cases need surgery within the first year, often soon after diagnosis. The main surgery is called a pull-through procedure. It removes the diseased bowel and connects the healthy part to the anus. The goal is to keep continence and normal bowel function while clearing the blockage. Different techniques exist, such as Swenson, Soave, and Duhamel. Each uses a slightly different method to remove and reconnect the bowel.
Modern Surgical Options
Today, surgeons often use minimally invasive or laparoscopic pull-through surgery. This reduces recovery time, scarring, and infection risk. In some centres, the operation is done entirely through the anus, called a transanal pull-through. No matter the method, the aim is to remove the diseased part and make sure the rest of the bowel works well.
When a child is very sick—due to enterocolitis, large bowel swelling, or poor nutrition—the surgery may happen in two steps. First, doctors create a diverting ostomy. They bring part of the healthy bowel to the surface of the abdomen to form a stoma (opening). This allows waste to exit into a colostomy bag. This gives the bowel time to heal while the child gains strength and better nutrition. Later, the pull-through surgery is done, and the ostomy is closed.
Care After Surgery
Post-surgical care is key in the treatment of Hirschsprung’s disease. Many children get back normal bowel habits. Some face problems like constipation, soiling, or enterocolitis. Constipation is common after surgery, especially if a short part of bowel still does not work well. Doctors usually manage this with diet changes, stool softeners, or bowel training under supervision.
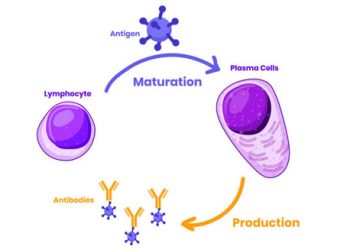
Another issue is Hirschsprung-associated enterocolitis. It can happen even after surgery. Parents learn to watch for warning signs such as fever, diarrhoea, and a swollen belly. They must seek care fast if these appear. Treatment includes antibiotics and rectal washes. In children with repeated episodes, preventive care may be needed.
Managing Ongoing Problems
Some children may soil or struggle with incontinence, which can be stressful. This often happens because of delayed toilet training or bowel movement issues, not due to surgery errors. Time, specialist care, and bowel programs usually help. Paediatric gastroenterologists and occupational therapists often guide families through this stage.
Rarely, when the first surgery fails or problems remain, doctors may need to do another surgery. This could mean removing more bowel or fixing the connection. Children with long-segment or total colonic disease often have harder recoveries. They might need extra feeding support or even intravenous nutrition in severe cases.
Long-Term Support and Monitoring
All children need regular check-ups after treatment of Hirschsprung’s disease. These visits track growth, bowel habits, and early signs of new issues. Some children benefit from emotional support, especially older kids who feel embarrassed about toileting.
Parents also need education. They must know how to care for the bowel, keep hygiene, and notice danger signs. Support groups and counselling can help families cope.
Families with a history of Hirschsprung’s disease may also need genetic counselling. This helps them understand the risk of having another child with the same problem and plan for early checks.
Future of Treatment
New research is looking at stem cell therapy and other methods that may work with or replace surgery. These treatments are not available yet, but they show promise for the future.
Conclusion
The treatment of Hirschsprung’s disease involves surgery, aftercare, regular follow-up, and family support. Most children recover well and live healthy lives. Still, ongoing care is important for problems like constipation or infections. Early and strong treatment makes a big difference in the quality of life for both child and family.