Hypoglycaemia is a serious condition. Yet, with the right knowledge, support, and treatments, most people live well while managing their risks. The outlook depends on how often and how severe the episodes are. It also depends on the person’s overall health and how quickly the condition is diagnosed and treated. If left untreated, hypoglycaemia can cause problems. However, education, regular monitoring, and good care can reduce or even prevent these risks.
In this section, we review the long-term outlook of hypoglycaemia. We look at factors that affect outcomes and how patients and healthcare providers can work together to improve quality of life.
General Prognosis for Hypoglycaemia
When caught early and treated well, hypoglycaemia usually has a good prognosis. Many people, especially those with type 1 or type 2 diabetes, learn to control their blood sugar and avoid dangerous lows. Education and proper treatment plans greatly lower the chance of severe or repeated episodes.
However, some people face a harder outlook. This includes those who have:
• Frequent severe hypoglycaemia episodes
• Hypoglycaemia unawareness (no warning signs)
• Untreated causes like insulinoma or adrenal problems
• Poorly controlled diabetes with unbalanced medication and lifestyle
These individuals face higher risks of memory loss, heart problems, injuries, and a lower quality of life. But with the right help, these risks can be lowered. Both patient and healthcare team must stay committed.
Prognosis in Diabetes-Related Hypoglycaemia
People with type 1 diabetes are at higher risk because they depend on insulin. They may face low blood sugar daily, especially during exercise, missed meals, or at night. Over time, repeated lows can dull their ability to sense warning signs. This is called hypoglycaemia unawareness.
Research shows that those with type 1 diabetes who adjust their lifestyle, use continuous glucose monitoring (CGM), and receive education can reduce episodes. Often, hypoglycaemia unawareness improves with better blood sugar control over weeks.
People with type 2 diabetes usually have a better outlook. Their blood sugar tends to be steadier. Reducing medication doses or switching to newer drugs like SGLT2 inhibitors or DPP-4 inhibitors can lower hypoglycaemia risk.
Prognosis in Non-Diabetic Hypoglycaemia
Non-diabetic hypoglycaemia patients fall into groups such as:
• Those with reactive hypoglycaemia after high-carb meals
• Those with fasting hypoglycaemia from hormonal or metabolic issues
• Rarely, those with insulin-producing tumours (insulinoma)
For most, prognosis is good once the cause is found. Dietary changes often control reactive hypoglycaemia. Treating the main disorder helps fasting hypoglycaemia. Surgery usually cures insulinoma symptoms.
Diagnosis can take time. Many live with unexplained symptoms for years. Early referral to an endocrinologist improves outcomes.
Prognosis in Children
Children with repeated hypoglycaemia, especially babies and toddlers, risk long-term effects if not treated fast. Glucose is crucial for brain growth. Prolonged lows can cause delays or learning problems.
But early diagnosis and good care help most children recover fully. Some outgrow causes tied to immature glucose control. Others with genetic or metabolic disorders may need lifelong care. Still, outcomes improve with medical advances and team care.
Prognosis in Older Adults
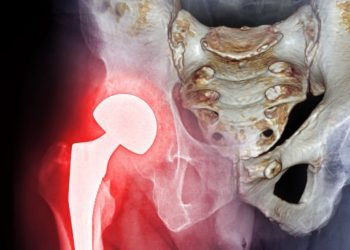
Older adults face higher risks from hypoglycaemia due to other illnesses like heart disease, kidney problems, or memory loss. Severe lows raise chances of falls, hospital stays, and even death.
Still, adjusting medications and aiming for safer blood sugar targets can improve safety. Doctors now focus on maintaining independence and life quality in older patients instead of strict glucose control.
Regular check-ups and medication reviews—especially for insulin or sulphonylureas—can prevent most episodes. Teaching families also helps monitor older adults.
Technological and Therapeutic Advances
Recent years brought big improvements for hypoglycaemia care. These include:
• Continuous glucose monitors (CGM) and flash sensors
• Insulin pumps that stop automatically when glucose is low
• “Artificial pancreas” systems that adjust insulin delivery
• New diabetes drugs that lower sugar without causing lows
• Apps and wearables for real-time alerts and trend tracking
These tools cut episode frequency, boost awareness, and help act before crises occur.
Importance of Long-Term Follow-Up
Ongoing care is vital to improve outlook. This means:
• Regular blood sugar and HbA1c tests
• Medication reviews
• Support for anxiety or fear related to hypoglycaemia
• Dietitian help for managing food triggers
• Specialist care for complex cases
Patients who work closely with their care teams and keep up monitoring tend to avoid complications and enjoy better lives.
Final Thoughts
Hypoglycaemia remains serious but the outlook is getting better. Modern treatments, tech, and education allow people—even those with complex needs—to avoid severe episodes and live fully. Early diagnosis, active management, and personalized care make this possible.
With more awareness and innovation, hypoglycaemia’s impact can lessen for all ages and groups.