Diagnosis of leg cramps begins with a thorough evaluation of a person’s symptoms, medical history, and lifestyle factors.
Leg cramps are common and usually harmless. Still, doctors must find out if cramps happen for no known reason (idiopathic) or show a deeper health problem. Early and accurate diagnosis of leg cramps helps create the best treatment plan and rules out serious issues like blood flow or nerve disorders.
Leg cramps can happen sometimes or often. Their pain ranges from mild discomfort to severe pain. In some people, cramps disturb sleep, exercise, or overall quality of life. Healthcare workers focus on telling apart harmless muscle cramps from those that need more medical care.
1. Detailed Patient History and Symptom Discussion
The first step in diagnosis of leg cramps is taking a detailed patient history. Doctors ask about how often cramps happen, how long they last, and how bad they feel. They also want to know when cramps usually appear—like at night or during activity. Learning which muscles hurt, if there are signs like tingling or numbness, and how long pain lasts helps with diagnosis.
Patients also share lifestyle habits such as hydration, exercise, diet, and any new medications. This information gives doctors a full picture of factors that may cause cramps.
2. Physical Examination and Functional Testing
Physical exams play an important role in diagnosis of leg cramps. The doctor checks muscle tone, strength, and flexibility in the painful leg or legs. They may feel the muscle for tenderness, swelling, or hardness. Seeing a cramp during the visit is rare but helpful.
Functional tests may include asking the patient to flex or extend their foot or walk on toes or heels. These tests check how muscles and nerves work. If reflexes, strength, or coordination seem off, doctors look deeper into nerve causes.
3. Reviewing Current Medications and Supplements
Reviewing medicines and supplements is key in diagnosis of leg cramps. Some drugs like diuretics, statins, beta-agonists, and certain blood pressure pills can cause muscle cramps as side effects. Overuse of common painkillers like ibuprofen or aspirin may also lower electrolytes and trigger cramps.
People should also discuss supplements, especially those with magnesium, calcium, or potassium. Both low and high levels of these minerals can affect muscles and cause cramps.
4. Blood Tests to Identify Underlying Issues
To check for metabolic or body-wide causes, doctors may order blood tests during diagnosis of leg cramps. These tests look for:
- Electrolyte imbalances (low potassium, calcium, or magnesium)
- Thyroid problems (low thyroid can increase cramps)
- Liver or kidney disease
- Vitamin shortages, especially B12 or D
- Blood sugar to check for diabetes or prediabetes
These results help find treatable causes and guide care.
5. Electromyography (EMG) and Nerve Conduction Studies
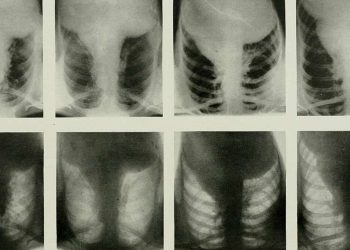
If leg cramps seem linked to nerve problems, more advanced tests may be needed. Electromyography (EMG) measures muscle electrical activity to check function and find issues. Nerve conduction tests check how well nerves send signals.
These tests are useful when symptoms include numbness, tingling, weakness, or if cramps relate to nerve diseases like peripheral neuropathy, multiple sclerosis, or spinal cord problems.
6. Imaging Scans to Investigate Structural Problems
Sometimes diagnosis of leg cramps needs imaging to check for structural issues causing nerve pressure or poor blood flow. Ultrasound can look at leg blood flow and detect peripheral artery disease. MRI or CT scans check for spine problems like herniated discs or spinal narrowing that may press on nerves and cause cramps.
These scans help rule out serious causes, especially if cramps last long, happen unevenly, or come with swelling or nerve symptoms.
7. Differential Diagnosis: Ruling Out Other Conditions
Many health issues can mimic or add to cramps, so diagnosis of leg cramps often means ruling out other conditions. These include:
- Restless legs syndrome: Often confused with cramps but causes a creeping discomfort.
- Claudication: Pain from poor blood flow during walking, sometimes mistaken for cramps.
- Deep vein thrombosis (DVT): A serious condition with calf pain and tightness.
- Muscle strain or tear: Causes pain that can feel like cramp soreness.
Knowing when, where, and how cramps happen helps tell these apart.
8. When to Refer to a Specialist
Most times, a general doctor can diagnose leg cramps. But if cramps last, get worse, or don’t respond to treatment, a specialist referral may be needed. Specialists may include neurologists, endocrinologists, or vascular surgeons. Referral is important if cramps come with warning signs like growing weakness, muscle loss, or bladder and bowel changes.
9. Monitoring and Follow-Up
After diagnosis of leg cramps, regular follow-up may be needed. This helps check if lifestyle or medicine changes work well. Patients might keep a “cramp diary” to note when cramps happen, how long they last, how bad they feel, and possible triggers.
This record helps doctors adjust treatment and catch any new symptoms early.
Summary
To summarise, diagnosis of leg cramps involves many steps starting with a full history and exam, and sometimes blood tests, nerve studies, or imaging. Finding the main cause is key to choosing the best treatment and stopping future cramps. With proper care, most people get relief and avoid problems from ongoing or bad leg cramps.