Diagnosis of Lipoedema can be particularly challenging because it is frequently misdiagnosed as obesity or lymphoedema.
The term diagnosis of lipoedema refers to a full medical check-up that helps identify this long-term condition. It mostly affects women and leads to uneven fat build-up, especially in the legs, thighs, and sometimes arms. Getting the diagnosis right early is very important. It helps start the right treatment plan, which reduces problems and improves life quality.
A proper diagnosis of lipoedema starts with taking a detailed health history. Doctors usually ask when symptoms began and if any family members had the same issue. They also want to know if hormonal changes—like puberty, pregnancy, or menopause—happened around the time symptoms appeared. These hormone shifts are key clues. Lipoedema often gets worse during these times.
Next, doctors ask how the condition affects walking or daily tasks. They also check for pain, easy bruising, or tenderness. This background information plays a big part in the overall diagnosis of lipoedema.
Physical Examination and Visual Signs
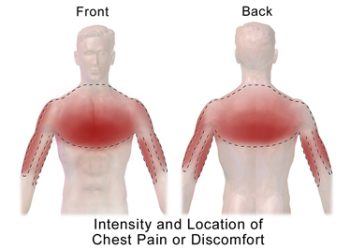
After gathering history, doctors do a full physical check. One clear sign of lipoedema is both legs growing larger in a balanced way. This is different from obesity. In lipoedema, the hands and feet usually look normal, creating a sharp line at the ankles or wrists.
The texture of the fat also feels different. It may seem rubbery or lumpy. People often say these areas hurt when touched and bruise easily. These are major signs that help with the diagnosis of lipoedema.
Doctors must also rule out other conditions. In lymphoedema, swelling often affects only one side and includes the feet. This doesn’t happen in lipoedema. Also, the fat in lipoedema doesn’t go away with diet or exercise. This makes it easier to tell it apart from obesity. Spotting these differences is an important part of diagnosing the condition.
Supporting Tests and Diagnostic Tools
There is no single blood test or scan made just for the diagnosis of lipoedema. Still, some tests can help doctors feel more confident in their decision.
Ultrasound can show fat structure and help rule out other problems. In tough cases, a scan called lymphoscintigraphy checks how the lymph system is working. These tests don’t confirm lipoedema but can support the diagnosis when used carefully.
One issue doctors face is that there are no worldwide standards for diagnosing lipoedema. This leads to confusion, late diagnoses, and added stress for patients. Luckily, more experts now follow trusted guidelines from groups like the Royal College of General Practitioners and the International Lipoedema Association. These help make the process clearer and more reliable.
Measurements, Referrals, and Mental Health
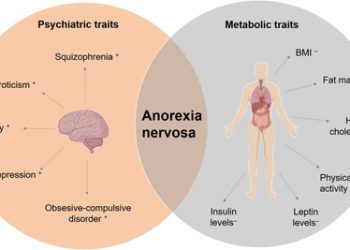
Sometimes, doctors take photos or measure limb sizes. These tools help track how the condition changes or how well treatments are working. Body Mass Index (BMI) and waist-to-hip ratios are also checked. But these numbers don’t tell the full story in lipoedema. Since fat is not spread evenly, these measurements are not reliable on their own. Still, they help rule out other problems like general obesity or metabolic issues.
It’s a good idea for patients to see a lipoedema expert or a team that includes skin, vein, and movement specialists. These professionals know how to spot subtle signs and create a full care plan. Their teamwork leads to a stronger diagnosis of lipoedema and better support going forward.
Emotional health is just as important. Because lipoedema changes how the body looks, it often causes anxiety, sadness, or body image struggles. Mental health professionals help people cope with these feelings during and after the diagnosis. Including them in the process makes the care more complete.
The Importance of Early and Accurate Diagnosis
To sum up, the diagnosis of lipoedema depends mostly on clinical judgement. Doctors need to know what signs to look for and how to rule out other causes. This process includes a full health history, careful physical exam, and sometimes imaging tests to support the findings.
Getting the diagnosis right, and doing it early, changes everything. It leads to better treatment results and helps ease both the physical discomfort and emotional strain linked with this condition.