Long QT syndrome (LQTS) is primarily caused by two types: inherited (congenital) and acquired. Both disrupt the heart’s electrical signaling, specifically affecting the ion channels that help repolarize the heart after each beat. Understanding these causes is crucial for identifying risks, offering genetic counseling, preventing sudden cardiac events, and guiding treatment strategies.
Inherited (Congenital) Causes
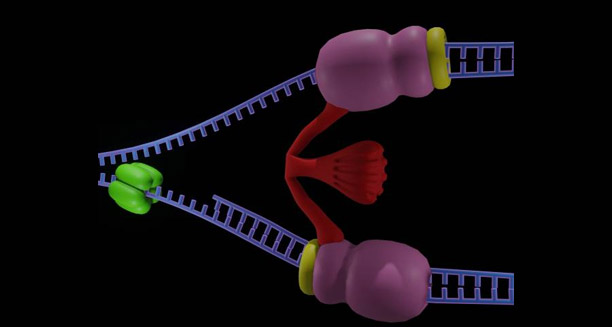
Inherited Long QT syndrome arises from mutations in genes that encode the proteins forming the heart’s ion channels, especially those controlling potassium, sodium, and calcium. These channels are vital for the heart’s electrical activity, and mutations lead to delayed repolarization or prolonged depolarization of the ventricular myocardium. As a result, the QT interval on the ECG becomes extended.
More than 17 genes are linked to congenital Long QT syndrome, but three main types account for most cases:
- LQT1: Caused by mutations in the KCNQ1 gene, affecting potassium flow. Triggers often include exercise, especially swimming.
- LQT2: Caused by mutations in the KCNH2 gene, also impacting potassium channels. Emotional stress or sudden noises are common triggers.
- LQT3: Linked to mutations in the SCN5A gene, affecting sodium channels. Arrhythmias typically occur during sleep or rest.
These genetic forms of Long QT syndrome follow an autosomal dominant inheritance pattern, meaning that a single mutated gene copy is sufficient to cause the disorder. Rare cases, such as Jervell and Lange-Nielsen syndrome, which also involves congenital deafness, inherit the condition in an autosomal recessive pattern, requiring both parents to carry the gene.
Variable Penetrance and Expressivity
An essential aspect of the causes of Long QT syndrome is variable penetrance and expressivity. Not all individuals with a genetic mutation will experience symptoms or prolonged QT intervals. Some may remain asymptomatic throughout life, while others may suffer from dangerous arrhythmias with minimal provocation. Environmental factors, age, sex hormones (particularly in females), and concurrent medical conditions can all influence the severity and presentation of the disease.
Acquired Causes of Long QT Syndrome
Unlike congenital forms, acquired Long QT syndrome occurs in people who don’t have a genetic predisposition but may develop prolonged QT intervals due to external triggers. Often, this type of LQTS is reversible once the underlying cause is identified and treated.
Drug-Induced Long QT Syndrome
One of the most common acquired causes is drug-induced Long QT syndrome, a significant concern in clinical medicine. Various medications can prolong the QT interval by interfering with cardiac ion channels, particularly those regulating potassium. These include:
- Antiarrhythmic drugs: Like sotalol, amiodarone, and quinidine.
- Antibiotics: Especially macrolides (e.g., erythromycin, clarithromycin) and fluoroquinolones (e.g., ciprofloxacin).
- Antidepressants and antipsychotics: Such as tricyclic antidepressants, SSRIs like citalopram, and antipsychotics like haloperidol.
- Antiemetics: Like ondansetron and domperidone.
- Opioids: Particularly methadone, especially when used in high doses or in combination with other QT-prolonging medications.
Polypharmacy (using multiple drugs that prolong the QT interval) is particularly dangerous for elderly patients or those with existing heart conditions.
Electrolyte Imbalances
Another key factor in acquired Long QT syndrome is electrolyte imbalances. Low levels of potassium (hypokalemia), magnesium (hypomagnesemia), or calcium (hypocalcemia) can impair the heart’s repolarization, prolonging the QT interval. These imbalances can result from diarrhea, vomiting, eating disorders, medications (like diuretics), or chronic kidney disease.
Other Acquired Causes
Other acquired causes of Long QT syndrome include:
- Bradycardia (slow heart rate): A prolonged pause between heartbeats can stretch the QT interval.
- Structural heart diseases: Conditions like cardiomyopathies and myocardial infarction (heart attack) can alter heart conduction.
- Endocrine disorders: Especially hypothyroidism, which can slow metabolism and impact cardiac repolarization.
- Starvation or malnutrition: Conditions like anorexia nervosa can alter electrolyte levels and cardiac function.
Genetic Predisposition and Triggers
Some individuals may have a genetic predisposition to Long QT syndrome, but the condition only manifests when triggered by an external factor, such as a drug or electrolyte imbalance. This is sometimes referred to as forme fruste Long QT syndrome, where genetic mutations become apparent only under specific circumstances.
Pregnancy and Postpartum Period
Pregnancy and the postpartum period are also high-risk times, particularly for women with LQT2. Hormonal changes can increase vulnerability to arrhythmias during these phases. Close monitoring and avoidance of known triggers are crucial during pregnancy and after childbirth.
Rare Causes: Neurological Events
In rare instances, neurological events like subarachnoid hemorrhage or traumatic brain injury can induce acquired Long QT syndrome. This may occur via autonomic nervous system dysfunction that disrupts the heart’s rhythm.
Conclusion: Multifactorial Causes
The causes of Long QT syndrome are multifactorial, involving both genetic mutations and environmental or iatrogenic triggers. While inherited forms require lifelong management, acquired types may be reversible with appropriate treatment. Early recognition and addressing the underlying causes are essential in preventing dangerous arrhythmias and sudden cardiac death in at-risk individuals and the general population.