Treatment of lung cancer involves a complex and carefully individualised approach, depending on the type, stage, location, genetic makeup of the tumour, and the overall health of the patient.
The main goal is to remove the cancer, shrink it, or keep it under control. Doctors also focus on easing symptoms and helping patients live longer and better. Medical science has come a long way. Today, people have more choices than ever before. Treatments now suit the needs of each patient much more closely.
Understanding the Type of Lung Cancer
The first step is to find out what kind of lung cancer a person has. Doctors group it into two main types—non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC).
NSCLC is more common and grows slowly. That gives doctors more options for how to treat it. SCLC is more aggressive. It often spreads early, so doctors use treatments that reach the whole body.
Surgery for Lung Cancer
Doctors may choose surgery to treat early-stage NSCLC. Surgery works best when the tumour is in one place and the patient is healthy enough for an operation. Common types of surgery include:
- Lobectomy: removing one full lobe of the lung (most common).
- Segmentectomy or wedge resection: removing a smaller lung section, often used for patients with weak lungs.
- Pneumonectomy: removing the entire lung, usually for large or central tumours.
After surgery, doctors may use chemotherapy or radiation to kill any cancer that remains. These extra steps lower the chance of the cancer returning.
Doctors do not usually use surgery for SCLC because it spreads too quickly.
Radiotherapy in Treatment of Lung Cancer
Radiation is a major part of the treatment of lung cancer. It works alone or alongside other methods. Doctors may use it:
- To cure early-stage cancer when surgery isn’t possible
- After surgery to kill leftover cells
- To ease symptoms like pain, bleeding, or blocked airways
A new form called stereotactic body radiotherapy (SBRT) gives strong, targeted doses in fewer sessions. This helps patients who cannot have surgery.
Chemotherapy and When It Helps
Chemotherapy plays a big role in lung cancer care, especially in SCLC and late-stage NSCLC. These drugs attack fast-growing cells and are given through the veins in cycles.
Doctors may give chemo:
- Before surgery (neoadjuvant) to shrink the tumour
- After surgery (adjuvant) to stop the cancer from coming back
- In advanced cases to ease symptoms and slow the disease
For SCLC, chemotherapy is usually the first step. Doctors often use two drugs together, like cisplatin and etoposide. It may not cure the cancer, but it can help with symptoms and improve life length.
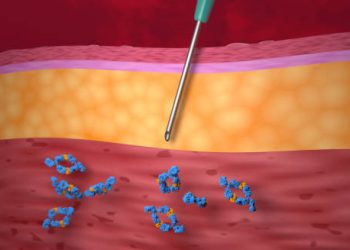
Targeted Therapy in Lung Cancer Care
Targeted therapy changed the treatment of lung cancer. These drugs focus on specific changes in cancer cells. They do not harm all fast-growing cells like chemo does.
Some examples are:
- EGFR inhibitors (e.g. erlotinib, gefitinib)
- ALK inhibitors (e.g. crizotinib)
- New drugs for ROS1, BRAF, and KRAS gene changes
Most of these are pills, not infusions. They often cause fewer side effects. These treatments work best in people who have certain types of cancer, like non-smokers with adenocarcinoma.
Immunotherapy: A New Direction
A newer and promising part of the treatment of lung cancer is immunotherapy. These drugs help the immune system fight the tumour.
Checkpoint inhibitors like nivolumab, pembrolizumab, and atezolizumab block cancer’s defense system. This allows immune cells to attack the tumour.
Immunotherapy works well in NSCLC with high PD-L1 levels. It can be used alone or with chemo. Some patients stay cancer-free long after treatment ends.
When Treatments Work Best Together
Often, doctors combine several types of treatment. Teams of specialists—including surgeons, oncologists, and radiologists—create a plan that suits each patient.
For example, a person with stage III NSCLC might get chemo and radiation together, followed by immunotherapy. In SCLC, chemo and radiation often go hand in hand. For advanced disease, doctors may also include immunotherapy.
Palliative Care in Treatment of Lung Cancer
When curing the cancer is not possible, palliative care becomes very important. The goal changes from cure to comfort. Doctors focus on making the patient feel better and improving daily life.
Palliative care includes:
- Treating pain
- Easing breathing with inhalers or draining fluid
- Giving food support
- Offering emotional care and end-of-life help
Some patients start palliative care early, while still getting other treatments. This approach helps the whole person, not just the disease.
Clinical Trials and New Options
Doctors are still finding new and better ways to treat lung cancer. Clinical trials test the latest drugs and treatments.
People with late-stage or hard-to-treat cancer may join trials to try these new therapies. While trials have risks, they also offer hope. Many of today’s best treatments came from past trials.
Lifestyle Changes and Support Programs
Along with medical care, lifestyle support helps in the treatment of lung cancer. Quitting smoking, eating well, and joining rehab programs can make a big difference.
Patients who stop smoking after diagnosis often respond better to treatment. They also face fewer problems.
Mindfulness, therapy, exercise, and support groups help patients cope better. These services improve mental health and daily strength.
A Changing Future in Lung Cancer Care
In summary, the treatment of lung cancer has many parts and keeps changing. From surgery and chemo to targeted and immune-based treatments, patients now have more hope than ever.
Early diagnosis, personalised care, and strong support systems give patients the best chance. The right mix of science and care can help people live longer and live well.