Causes of Giant Cell Arteritis
The causes of giant cell arteritis are still being researched. However, current evidence suggests that a combination of genetic, environmental, and immunological factors is involved. Doctors consider giant cell arteritis an autoimmune condition in which the immune system mistakenly attacks artery walls, causing inflammation and narrowing of the vessels.
Understanding the underlying mechanisms helps in identifying at-risk individuals and developing better treatments. The condition is most common in older adults, especially women over 50, but doctors still do not fully understand what triggers the disease.
Immune System Dysfunction
The leading theory is that giant cell arteritis arises from immune dysregulation, where immune cells misidentify healthy tissue—in this case, artery walls—as harmful. This sets off a chronic inflammatory response.
Key immune cells involved include:
CD4+ T lymphocytes
Macrophages
Giant cells are large immune cells formed when multiple macrophages fuse together
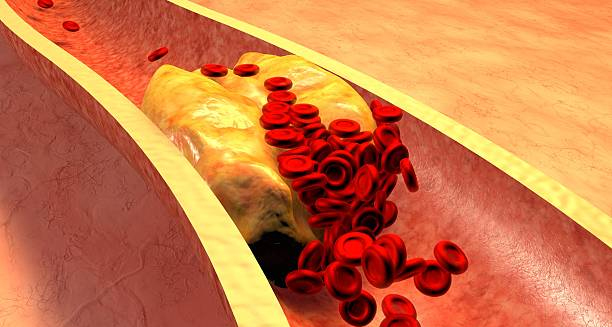
These cells infiltrate the tunica media and adventitia (layers of the arterial wall), forming granulomas and releasing inflammatory cytokines. The inflammation leads to:
Thickening of the artery wall
Narrowing or obstruction of the blood vessel
Potential tissue damage due to reduced blood flow
This explains the classic symptoms of ischaemia, such as headache, jaw pain, and vision disturbances.
Genetic Predisposition
There is a strong genetic component to giant cell arteritis. Studies have found that people with certain variations in the HLA (human leukocyte antigen) system, particularly HLA-DRB1*04, are more likely to develop the condition.
While having these genes does not guarantee disease, it increases susceptibility, particularly when combined with environmental or age-related factors. Family history may also influence the risk, although doctors do not consider GCA a hereditary disease in the traditional sense.
Ageing and Vascular Changes
Ageing is the strongest risk factor for developing giant cell arteritis. The vast majority of cases occur in people over 50, and risk increases steadily with age.
Several theories explain this age-related risk:
Ageing causes degeneration of vascular structures, making them more vulnerable to inflammation
The immune system becomes more prone to autoimmune activation
Arterial elasticity declines, contributing to vascular stress and damage
The intersection of these factors creates a favourable environment for GCA to develop.
Environmental Triggers
Doctors suspect that certain environmental factors may trigger the initial immune response in individuals who are predisposed. These may include:
1. Infections
Viral or bacterial infections have long been hypothesised as potential triggers. Though no single pathogen has been definitively identified, several candidates include:
Parvovirus B19
Varicella zoster virus (VZV)
Chlamydia pneumoniae
These pathogens may provoke an immune response that cross-reacts with arterial tissues, leading to autoimmunity. Some studies have found fragments of viral DNA in the arteries of patients with GCA, although evidence remains inconclusive.
2. Seasonal Variations
Epidemiological data suggest a seasonal pattern to disease onset, with more diagnoses occurring during colder months. This may point to a link with seasonal infections or reduced sunlight exposure, although the exact relationship is unclear.
3. Geographic Trends
Giant cell arteritis is more common in certain regions, particularly:
Northern Europe and Scandinavia
North America
Parts of Australia and New Zealand
This geographic distribution supports both genetic and environmental influences, including climate, infection exposure, and possibly vitamin D levels.
Coexisting Conditions
Giant cell arteritis often occurs in conjunction with polymyalgia rheumatica (PMR), an inflammatory condition that causes stiffness and pain in the shoulders and hips. Up to 50% of patients with GCA also have symptoms of PMR.
This association suggests shared inflammatory mechanisms, possibly involving overlapping genetic susceptibility and immune pathways.
Gender Differences
Giant cell arteritis affects women more often than men, with a female-to-male ratio of approximately 2:1 to 3:1. The reasons for this are not fully understood but may involve:
Hormonal influences on immune regulation
Differences in vascular structure or immune gene expression
Postmenopausal women are particularly at risk, further implicating hormonal changes as a contributing factor.
Conclusion
While the exact causes of giant cell arteritis remain under investigation, current research points to a multifactorial process involving:
Immune system malfunction
Genetic predisposition
Age-related vascular changes
Possible environmental triggers
Causes of Giant Cell Arteritis
Identifying and understanding these factors is crucial for early detection and better management of this potentially sight-threatening disease.