Causes of Granulomatosis with Polyangiitis
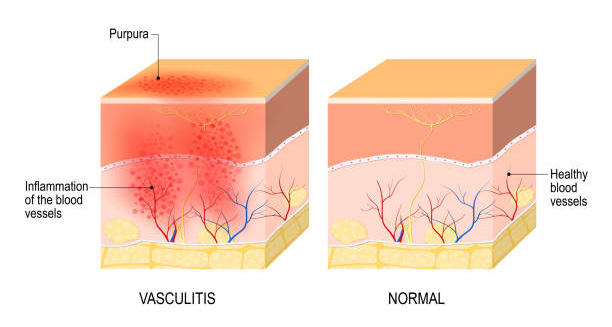
Doctors still do not fully understand what causes granulomatosis with polyangiitis (GPA). However, they believe it begins with an abnormal immune response that causes inflammation in blood vessels and nearby tissues. Even though the exact cause remains unknown, research points to a mix of genetics, environmental exposure, infections, and autoimmune activity as major contributors.
GPA belongs to a group of illnesses called ANCA-associated vasculitides, which involve harmful antibodies called anti-neutrophil cytoplasmic antibodies (ANCAs). These antibodies seem to play a key role in the damage seen in affected organs.
1. Autoimmune Mechanisms
First and foremost, GPA behaves like an autoimmune disease. In this condition, the immune system attacks the body’s own tissues by mistake. While the reason for this faulty immune attack isn’t clear, several things happen:
- ANCAs target specific proteins inside white blood cells (neutrophils), mainly proteinase 3 (PR3) or myeloperoxidase (MPO)
- These activated neutrophils release harmful substances
- These substances damage blood vessels and nearby tissues
This process creates granulomas, blood vessel inflammation (vasculitis), and in some cases, tissue death (necrosis).
1. Autoimmune Mechanisms
First and foremost, GPA behaves like an autoimmune disease. In this condition, the immune system attacks the body’s own tissues by mistake. While the reason for this faulty immune attack isn’t clear, several things happen:
- ANCAs target specific proteins inside white blood cells (neutrophils), mainly proteinase 3 (PR3) or myeloperoxidase (MPO)
- These activated neutrophils release harmful substances
- These substances damage blood vessels and nearby tissues
This process creates granulomas, blood vessel inflammation (vasculitis), and in some cases, tissue death (necrosis).
2. Genetic Factors
Although GPA doesn’t pass directly from parent to child, certain genes may make some people more likely to develop it. For example:
- Variations in HLA-DP, HLA-DQ, and HLA-DR genes increase the risk
- Other genes such as PTPN22 and SERPINA1 affect how the immune system works
- People with a family history of autoimmune diseases like lupus or rheumatoid arthritis may face a slightly higher risk
These genetic factors suggest that some individuals carry an inherited vulnerability. When exposed to the right trigger, their immune system may overreact.
3. Environmental and Occupational Exposures
Next, environmental and workplace exposures may also trigger GPA in people who already carry genetic risk. Research has linked the disease to:
- Silica dust, especially in mining and construction
- Solvents, paint fumes, and industrial chemicals
- Farming and agricultural chemicals
These substances may damage tissues or overstimulate the immune system, leading to inflammation.
4. Infections
Infections may also play an important role. They can either trigger GPA for the first time or make it worse later. Specifically:
- Staphylococcus aureus, a bacteria that often lives in the nose, may keep the immune system constantly active
- Viruses such as hepatitis, Epstein-Barr virus, or others might confuse the immune system and cause it to attack healthy tissues
These infections may set off or maintain harmful immune reactions that damage the blood vessels.
5. Drug-Induced Triggers
Although uncommon, certain medications can cause a condition that looks like GPA. These include:
- Hydralazine (used for high blood pressure)
- Propylthiouracil (PTU) (used for thyroid problems)
- Cocaine contaminated with a chemical called levamisole
Usually, the symptoms go away after stopping the drug. Doctors can often tell drug-induced cases apart from true GPA through blood tests and history.
6. Immune System Triggers
Sometimes, GPA may start after the immune system reacts to injury or repeated exposure to certain antigens. For example:
- Tissue damage may release signals that trigger the immune system
- Chronic stimulation from unknown microbes or environmental triggers may push immune cells to act abnormally
- T cells, B cells, and neutrophils then create a cycle of inflammation that keeps damaging blood vessels
This overreaction turns into chronic inflammation unless doctors stop it early.
7. Hormonal and Biological Factors
Finally, some differences in age, sex, and hormones may affect who gets GPA. For instance:
- Middle-aged men seem to have a slightly higher risk
- Hormonal changes might influence how the immune system behaves
- Age-related changes in immunity may explain why GPA usually appears in adults
Although doctors don’t yet understand these patterns fully, they point to a mix of biological influences.
Summary of Contributing Factors
| Category | Examples |
|---|---|
| Autoimmune response | ANCA antibodies, neutrophil activation |
| Genetic susceptibility | HLA genes, PTPN22, SERPINA1 |
| Environmental exposure | Silica, solvents, farm chemicals |
| Infections | Staphylococcus aureus, viral infections |
| Drug-induced triggers | Hydralazine, PTU, levamisole |
| Biological factors | Age, sex, immune system behavior |
Multifactorial Nature of GPA
So far, no single cause explains all cases of GPA. Instead, the disease likely results from a mix of factors, such as:
- A person’s genetic makeup
- Exposure to a trigger, like a chemical or infection
- A resulting immune system reaction that spirals out of control
This complex picture explains why GPA looks different from one person to another. It also guides doctors to treat the root immune problem—not just the symptoms.
Conclusion | Causes of Granulomatosis with Polyangiitis
To sum up, GPA results from a combination of genetic, environmental, infectious, and immune-related factors. Even though researchers haven’t found one clear cause, growing evidence points to autoimmune activity driven by ANCAs. By better understanding what causes GPA, doctors can improve how they diagnose it, treat it, and support patients living with this rare but serious condition.