The causes of hidradenitis suppurativa (HS) are complex and involve a mix of genetic, immune, hormonal, and environmental factors. While the exact cause is still not fully understood, research shows that HS begins with an inflammatory reaction in hair follicles. This condition is not caused by poor hygiene or infection, although these are common misconceptions. Instead, HS is a chronic skin disorder driven by internal processes that lead to inflammation, swelling, and tissue damage.
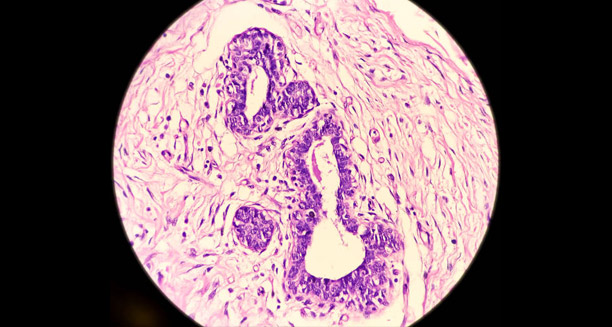
Follicular Occlusion: The Starting Point
At the core of HS is follicular occlusion, which means the hair follicle becomes blocked. In people with HS, follicles—especially in areas like the underarms, groin, buttocks, and under the breasts—get clogged with keratin or debris. This blockage traps sweat and oil inside the follicle. Eventually, the follicle bursts, releasing its contents into the surrounding skin. This triggers a strong immune response that leads to swelling, pus, abscesses, and ultimately scarring.
Genetics and Family History
Genetics plays a significant role in HS. About one in three to four people with HS has a close relative with the condition. This points to a strong hereditary link. Some studies have found mutations in genes involved in gamma-secretase, an enzyme that affects skin and follicle health. However, not all patients have these mutations, suggesting that multiple genes may be involved.
Immune System Overactivity
HS is also linked to immune system dysregulation. Many patients show an exaggerated inflammatory response to minor skin damage. This includes an overproduction of immune proteins like TNF-alpha and interleukin-1 (IL-1). These substances drive ongoing inflammation, attracting more immune cells to the area and leading to further damage and chronic flare-ups.
Hormonal Factors
Hormones influence the onset and severity of HS. The condition usually starts after puberty and is more common in women of reproductive age. Hormonal changes during menstruation, pregnancy, or menopause can affect symptoms. Some women notice a flare-up before their period, while others find relief during pregnancy. Treatments that alter hormone levels, such as birth control pills or anti-androgens, can help in some cases.
Obesity and Skin Friction
Being overweight is a well-known risk factor for HS. Skin folds, moisture, and friction can make symptoms worse. In addition, obesity is linked to chronic low-level inflammation, which can worsen the condition. Weight loss has been shown to reduce flare-ups and improve outcomes for many patients.
Smoking
Smoking is one of the strongest lifestyle risk factors for HS. Nicotine affects both the immune system and sweat glands. It also interferes with wound healing and increases the chance of follicle blockage. Because of its impact, quitting smoking is often a top priority in HS treatment plans.
Role of Bacteria
Although bacteria are not the cause of HS, they can worsen the condition after lesions form. Bacteria can colonise open wounds, increasing pain, odour, and drainage. In some cases, this may lead to secondary infections. However, these are typically a result of the disease rather than its cause.
Stress and Emotional Health
Chronic stress doesn’t cause HS but can certainly make it worse. Stress can affect hormone levels and disrupt the immune system, leading to more frequent or severe flare-ups. Mental health support, stress-reduction techniques, and therapy may be valuable parts of treatment.
Associated Conditions
HS has also been linked to other medical conditions, including Crohn’s disease, polycystic ovary syndrome (PCOS), and metabolic syndrome. These links support the idea that HS is not just a skin condition, but part of a broader systemic disorder. Treating these underlying conditions can improve HS outcomes.
Conclusion
Hidradenitis suppurativa is a multifactorial disease, meaning it results from the combined effects of genes, immune function, hormones, and lifestyle. Understanding these root causes helps patients and healthcare providers focus on what really matters—early diagnosis, effective treatment, and long-term disease control. By moving away from outdated myths and focusing on evidence-based care, it is possible to improve both symptom control and quality of life for people with HS.