Male menopause, also called andropause or late-onset hypogonadism, primarily results from the gradual decline in testosterone levels that begins in midlife. Unlike the abrupt hormonal changes women experience during menopause, the drop in testosterone in men happens slowly. Understanding the causes of male menopause is key to diagnosis and effective management.
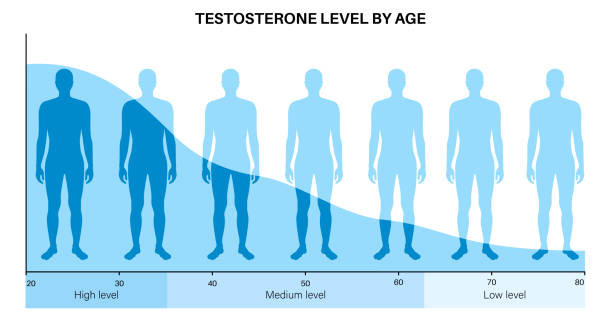
While testosterone levels typically decrease by about 1% per year after age 30 or 40, not every man develops symptoms. When symptoms do appear, other factors often accelerate or worsen hormonal decline. Below are the main causes contributing to male menopause:
Age-Related Decline in Testosterone Production
The fundamental cause is natural ageing. Leydig cells in the testes gradually produce less testosterone over time. Additionally, the hypothalamic-pituitary-gonadal (HPG) axis—which regulates hormone production—becomes less efficient. The hypothalamus signals the pituitary gland less effectively to release luteinising hormone (LH), reducing testosterone stimulation from the testes.
Some men tolerate lower testosterone without symptoms, while others are more sensitive to even small declines. Genetics, lifestyle, metabolic health, and overall resilience influence this variation.
Chronic Illnesses and Medical Conditions
Several chronic diseases are linked to lower testosterone and may worsen male menopause symptoms:
- Type 2 diabetes, obesity, and metabolic syndrome: Insulin resistance and high blood sugar disrupt hormonal balance. Fat cells, especially abdominal fat, convert testosterone into estrogen via the enzyme aromatase, lowering available testosterone.
- Cardiovascular disease
- Chronic kidney and liver disease
- HIV/AIDS
- Cancer and cancer treatments: Chemotherapy or radiation affecting the testes or brain
- Inflammatory conditions: Rheumatoid arthritis
- Sleep apnoea: Common in ageing men, significantly lowers testosterone by disrupting sleep quality
Lifestyle-Related Causes
Modern lifestyle habits can accelerate testosterone decline:
- Poor diet: Deficiencies in zinc, vitamin D, magnesium, and healthy fats impair hormone production.
- Lack of physical activity: Sedentary behaviour leads to muscle loss and weight gain, negatively impacting testosterone.
- Excess alcohol: Heavy drinking disrupts hormone metabolism and liver function.
- Drug use: Recreational drugs, including marijuana and opioids, suppress testosterone.
- Smoking: Tobacco impairs circulation and hormone production.
- Chronic stress: Elevated cortisol from stress directly inhibits testosterone production and contributes to anxiety, fatigue, and sleep problems.
Lifestyle changes can often improve testosterone levels and reduce symptoms without medication.
Psychological and Emotional Stressors
Emotional wellbeing influences testosterone levels in both directions. Major life changes such as retirement, divorce, financial strain, or loss of loved ones increase stress and suppress testosterone. Depression and anxiety also disrupt the HPG axis.
Chronic stress can create a vicious cycle: stress lowers testosterone, which worsens mood and energy, causing more stress. Recognizing this relationship is vital for effective care.
Medication-Related Causes
Certain medications interfere with testosterone production or mimic male menopause symptoms:
- Corticosteroids (e.g., prednisone)
- Opioid painkillers
- Some antidepressants
- Chemotherapy drugs
- Anti-androgens for prostate cancer
- Beta-blockers and diuretics
- Anabolic steroids and some over-the-counter supplements
If symptoms start after medication changes, patients should consult their doctor about alternatives or dosage adjustments.
Environmental Toxins and Endocrine Disruptors
Exposure to chemicals that disrupt hormone function is a growing concern and may contribute to declining testosterone:
- Plastics containing bisphenol A (BPA)
- Phthalates in cosmetics and personal care products
- Pesticides and herbicides in food and water
- Heavy metals like lead and mercury
Reducing exposure by using glass or stainless-steel containers, eating organic foods, and avoiding chemical-heavy products may support hormonal health.
Genetic Predisposition
While most male menopause cases are linked to lifestyle or environmental factors, genetics can play a role. Conditions such as Klinefelter syndrome, hemochromatosis, or congenital hypogonadism cause lifelong testosterone deficiencies that worsen with age. A family history of early-onset andropause or hormonal disorders may increase risk.
Although genetics cannot be changed, awareness enables early testing and management.
Summary
The causes of male menopause are multifactorial. Ageing is the primary driver, but chronic illness, lifestyle, psychological stress, medications, environmental toxins, and genetics all contribute. Understanding these factors empowers men to take proactive steps for hormonal health. In many cases, targeted interventions and lifestyle improvements can alleviate or prevent symptoms.