The causes of malignant brain tumour are not fully understood. Most cases develop without a clear reason. However, research shows that certain genetic, environmental, and lifestyle factors may increase risk.
While some tumours are linked to inherited genes or prior radiation, many result from complex interactions between a person’s DNA and their surroundings over time.
Understanding these causes is vital. It helps with early detection, guides targeted treatment, and improves survival. This section explores known and suspected contributors to malignant brain tumour development.
Genetic Mutations and Inherited Syndromes
Genetic mutations are a major cause of malignant brain tumours. These mutations can be inherited or acquired during a person’s life.
1. Inherited Genetic Syndromes
Some rare inherited disorders increase brain cancer risk. These include:
- Li-Fraumeni syndrome – caused by mutations in the TP53 gene; linked to gliomas and medulloblastomas.
- Neurofibromatosis type 1 and 2 (NF1/NF2) – raises the risk of gliomas, schwannomas, and ependymomas.
- Turcot syndrome – tied to colorectal cancer and high-grade gliomas due to APC or mismatch repair gene mutations.
- Tuberous sclerosis complex – leads to benign and malignant tumours in the brain and other organs.
These conditions show how faulty tumour-suppressor genes and oncogenes can drive tumour growth.
2. Acquired Genetic Alterations
Most brain tumours occur from random mutations, not inherited ones. These may arise from DNA replication errors, oxidative stress, or environmental exposure. Common tumour-related mutations include:
- EGFR amplification – common in glioblastoma; drives aggressive growth.
- IDH1/IDH2 mutations – found in low-grade gliomas; linked to better outcomes.
- 1p/19q co-deletion – seen in oligodendrogliomas; improves response to treatment.
- MGMT promoter methylation – predicts better response to alkylating chemotherapy.
Exposure to Ionising Radiation
Ionising radiation is one of the few confirmed environmental causes of malignant brain tumour. Exposure may happen through:
- Radiation therapy in childhood
- Nuclear accidents or occupational exposure
- Frequent high-dose imaging procedures
Radiation can damage DNA and cause mutations. Children are especially vulnerable due to their developing brains and longer lifespan.
Importantly, non-ionising radiation, like that from mobile phones or Wi-Fi, has not been proven to cause brain tumours. Large studies such as INTERPHONE and the UK Million Women Study found no consistent link.
Immunosuppression and Organ Transplants
People with weakened immune systems have a higher risk of developing brain lymphomas, especially primary central nervous system lymphoma (PCNSL). High-risk groups include:
- People living with HIV/AIDS (especially with low CD4 counts)
- Organ transplant recipients on immunosuppressants like cyclosporine
- Autoimmune disease patients on long-term immunosuppressive therapy
Weakened immunity may reduce the body’s ability to destroy abnormal cells or control latent viruses like Epstein-Barr virus (EBV).
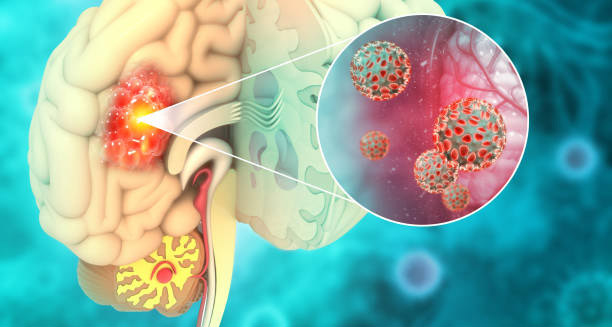
Viral Infections
Some viruses may play a role in tumour development. Although evidence is still evolving, studies suggest:
- Epstein-Barr virus (EBV) – linked to CNS lymphomas in immunocompromised patients
- Cytomegalovirus (CMV) – found in some glioblastoma samples, though its role remains unclear
- Polyomaviruses (e.g., SV40) – once suspected due to vaccine contamination, but no proven link exists
Research is ongoing to determine how viruses may affect tumour formation or growth.
Environmental and Occupational Exposures
There is no single toxin proven to cause brain cancer, but some occupational exposures raise concern. These include:
- Solvents and pesticides – used in farming, painting, or factory work
- Heavy metals – like lead or arsenic
- Petrochemical exposure – among oil, rubber, or plastic industry workers
- Healthcare radiation – radiologists and nurses may receive repeated low-level exposure
Long-term or repeated contact with harmful substances, combined with genetic risk, may increase cancer risk.
Hormonal and Gender Differences
Hormones may influence the risk of malignant brain tumour:
- Oestrogen receptors are found in some gliomas, suggesting a possible role in tumour behaviour.
- Males are slightly more likely to develop glioblastoma, but the reason remains unclear.
These gender-related differences are still being studied.
Age and Ageing
The risk of malignant brain tumours rises with age, especially after 45. This may be due to:
- Accumulated DNA damage
- Weakened cell repair systems
- Changes in gene expression and telomere shortening
Older adults are more likely to develop fast-growing gliomas with poorer outcomes.
Traumatic Brain Injury (TBI)
Head injuries, including concussions, do not cause malignant brain tumours. Despite early theories, large-scale studies have not found a consistent link between trauma and tumour formation.
Mobile Phones and EMF Exposure
The possible link between mobile phone use and brain tumours remains controversial. However:
- Studies like INTERPHONE, the Danish Cohort, and the Million Women Study have found no strong evidence of increased risk.
- No biological mechanism has been proven.
- Ongoing research continues as mobile phone use increases.
Lifestyle and Diet
Unlike other cancers, lifestyle choices have little proven impact on brain tumour risk:
- Smoking may lead to lung cancer, which can spread to the brain, but doesn’t cause brain tumours directly.
- Alcohol, obesity, and diabetes are linked to general cancer risk, but not brain tumours specifically.
- High nitrate diets (e.g., processed meats) have been studied, but findings are unclear.
That said, a healthy lifestyle still supports overall wellbeing and recovery.
Summary
The causes of malignant brain tumour are complex. They involve a mix of genetics, environment, immune health, and ageing. Some risk factors, like inherited mutations or radiation, are known. Others—like viral infections or chemical exposure—are still being researched.
In many cases, the exact cause is never found. But as science progresses, better understanding may lead to earlier detection, safer prevention, and more precise treatments.