Causes of Mastocytosis
Understanding the Causes of Mastocytosis is critical for clinicians, researchers, and patients alike, as it offers insight into how and why this rare disorder develops. The Causes of Mastocytosis are primarily rooted in genetic mutations that affect the growth and behaviour of mast cells—immune system cells involved in allergic reactions and inflammation. These mutations result in the accumulation of mast cells in the skin, bone marrow, liver, spleen, and other tissues, leading to a range of symptoms depending on the organs affected.
The Role of the KIT Gene in Mastocytosis
At the centre of most cases of mastocytosis is a change in the KIT gene. This gene makes a protein called KIT receptor tyrosine kinase. This receptor sits on the surface of mast cells and helps control how they grow, develop, and stay alive. Normally, KIT only turns on when it binds with a molecule called stem cell factor (SCF). But in mastocytosis, a common change—called the D816V mutation—makes KIT stay active all the time. This causes mast cells to grow too much and build up in tissues.
Doctors have found this D816V mutation in over 90% of adults with systemic mastocytosis. Many children with cutaneous mastocytosis also have it. Since this mutation happens after birth, people don’t inherit it. Even so, researchers are still looking into whether some people may carry inherited changes that increase their risk of mast cell problems.
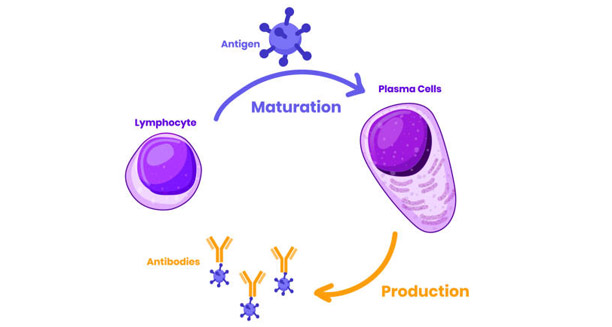
Immune System Imbalance and Overgrowth
The Causes of Mastocytosis don’t stop with genetic changes. Sometimes, the immune system may not work properly, especially in children who don’t have the KIT mutation. In these cases, scientists believe other signals in the body may push mast cells to grow too much. For example, higher levels of chemicals like interleukin-6 (IL-6) and tumour necrosis factor-alpha (TNF-α) may create an environment that encourages mast cell buildup.
Mast cells also affect their surroundings by releasing chemicals like histamine, tryptase, and prostaglandins. In mastocytosis, this becomes a harmful loop. The more mast cells there are, the more signals they send out, which leads to even more mast cell growth and survival.
Types of Mastocytosis and What Triggers Symptoms
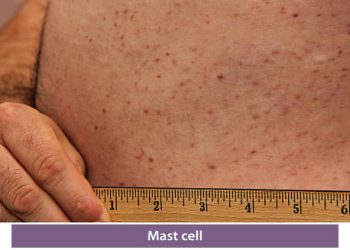
Doctors split mastocytosis into two main types: cutaneous and systemic. In cutaneous mastocytosis, extra mast cells only appear in the skin. In systemic mastocytosis, they spread to organs like the bone marrow, liver, and spleen. The Causes of Mastocytosis can vary slightly between these types, especially when comparing adults to children.
In children, mastocytosis often shows up in the first two years of life and usually stays limited to the skin. Most of the time, it gets better or even goes away with age. The cause in these young cases isn’t always clear, especially when no KIT mutation is found. On the other hand, adults are more likely to develop systemic mastocytosis. These cases often link to the D816V mutation and tend to be long-lasting or get worse over time. This is especially true in aggressive forms or when it becomes mast cell leukaemia.
Some things don’t cause mastocytosis but can make symptoms worse. These triggers include:
- Hot or cold temperatures, pressure, or friction
- Strong emotions or stress
- Certain medicines like NSAIDs, antibiotics, or painkillers
- Alcohol and some foods like aged cheese, shellfish, or vinegar
- Infections or changes in hormones
Recognising these triggers helps people manage the disease better.
Rare Genetic Links and Related Conditions
In rare cases, people may inherit a higher chance of developing mastocytosis. Although familial mastocytosis is very uncommon, a few studies suggest that it can run in families. Sometimes, mastocytosis also shows up alongside blood disorders like myelodysplastic syndromes (MDS) or chronic eosinophilic leukaemia. Doctors think these diseases might share similar genetic or cellular mistakes.
There’s also a condition called mast cell activation syndrome (MCAS). In MCAS, people have severe mast cell symptoms but don’t have extra mast cells. Even though mastocytosis and MCAS are different, their symptoms and causes can overlap in some cases.
How Molecular Pathways Influence the Causes of Mastocytosis
New research is diving deeper into how different cell signals affect mast cell growth. Apart from the KIT pathway, scientists are studying other systems like PI3K/AKT/mTOR, JAK/STAT, and RAS/MAPK. These systems help cells grow and respond to threats. If they go wrong, they may help the disease spread or resist treatment.
Because of this, newer treatments now target these exact problems. Drugs like midostaurin and avapritinib are designed to block KIT mutations. These medicines mark a big step forward in treating hard-to-manage or advanced systemic mastocytosis.
Summary of the Causes of Mastocytosis
In summary, the Causes of Mastocytosis mainly involve changes in the KIT gene, especially the D816V mutation. This change causes mast cells to grow too much and collect in tissues. But there’s more to the story. Immune system problems, triggers from the environment, and rare genetic links also play a part. Adult cases often involve the whole body and tend to last longer. In contrast, many childhood cases stay in the skin and get better over time.
Ongoing studies are bringing hope. They continue to uncover how mast cells behave and how we can stop them. These discoveries are leading to better treatments and improving life for people with this rare disease.