The complications of low sperm count extend far beyond an inability to conceive.
Infertility is the most obvious and immediate result. But the emotional, mental, and even physical effects can greatly harm a man’s health and quality of life. Knowing these complications early helps in getting the right medical and emotional help.
Infertility and Related Problems
The main complication of low sperm count is male infertility. Infertility means not being able to conceive after 12 months of regular, unprotected sex. A sperm count below 15 million per millilitre of semen lowers the chance of natural pregnancy. For some men, low count comes with poor movement (motility) or abnormal shape (morphology) of sperm. This makes it harder for sperm to reach and fertilise the egg. Even if sperm are present, their ability to work well may be too weak for pregnancy without medical help.
Emotional and Psychological Impact
The effects of low sperm count go beyond the body. The emotional toll can be deep. Men who learn they are infertile may feel:
- Low self-esteem
- Depression
- Anxiety
- Anger or guilt
- Relationship strain or isolation
In many cultures, fatherhood is tied to masculinity. This can make feelings of failure stronger. Men may feel less “manly” even though infertility is a medical issue affecting millions worldwide. Stigma often stops men from talking about the problem or seeking help, which can delay treatment and add stress.
Relationship Strain
Fertility issues can also cause problems between partners. Couples may face poor communication, sexual anxiety, blame, or resentment. The stress of repeated negative pregnancy tests or failed treatments can create distance and mistrust. Even when couples use donor sperm, adoption, or surrogacy, the emotional weight may stay if the root cause is not addressed.
Financial Burden of Treatment
Another serious complication of low sperm count is the cost of diagnosis and treatment. Finding the cause often needs many tests — semen analysis, hormone checks, genetic screening, and sometimes imaging. Private testing can be costly. If assisted reproduction like IVF or ICSI is needed, expenses can rise sharply. Multiple attempts may be needed, with no guarantee of success. For many couples, these costs add to the stress and sometimes stop them from getting treatment at all.
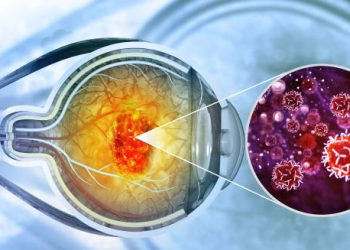
Medical Risks and Hidden Conditions
Low sperm count can also be a warning sign for other health issues, such as:
- Low testosterone or other hormone problems
- Genetic disorders like Klinefelter syndrome or Y-chromosome changes
- Testicular tumours or damage
- Chronic illnesses like diabetes, kidney disease, or liver problems
- Pituitary gland disorders
Finding low sperm count early can reveal these problems and allow treatment before they get worse. Fertility checks can sometimes open the door to better overall health care.
Invasive Procedures and Risks
Men with very low sperm count or no sperm at all may need surgical sperm retrieval methods like TESE or micro-TESE. These surgeries have risks, including bleeding, infection, testicular damage, and sometimes infertility from scarring.
Genetic Concerns
When pregnancy happens through ART despite low sperm count, there may be a risk of passing on infertility. Some genetic causes, like Y-chromosome deletions, can be inherited if ICSI is used. This makes genetic counselling important before trying for a baby.
Long-Term and Social Impact
Couples who stay childless may face social exclusion, especially where parenthood is highly valued. This can affect self-worth, social life, and even care in old age. Feelings of regret or loss can last for years, making emotional support vital.
Public Health Considerations
Low sperm count is also being studied as a public health issue. Research shows falling sperm counts in many parts of the world. Factors like hormone-disrupting chemicals, pollution, and stress may play a role. This trend suggests many individual cases could be part of a wider health problem.
Final Thoughts on the Complications of Low Sperm Count
The complications of low sperm count cover medical, emotional, financial, and social areas. While infertility is central, it is only one part of the story. Early checks, kind medical care, mental health support, and honest talks between partners are key. As treatments improve, options for men are growing. But managing the emotional side is just as important as the physical side.