Diagnosis and Evaluation of Brain Abscess
The diagnosis and evaluation of brain abscess requires prompt medical attention, as symptoms can worsen quickly. Since the clinical signs often resemble those of other neurological conditions, imaging and lab tests are essential in confirming the diagnosis.
5 Methods of Diagnosis and Evaluation of Brain Abscess
1. Clinical assessment
Doctors first conduct a thorough medical history and neurological exam. They assess for headache, fever, neck stiffness, confusion, and focal neurological deficits such as weakness or vision problems.
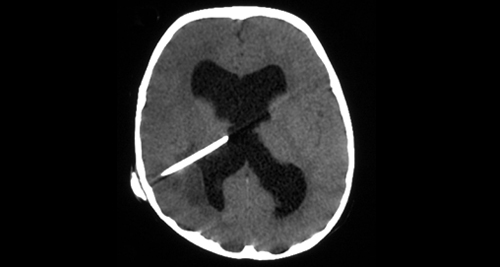
2. Imaging studies
- CT scan with contrast: This is often the first diagnostic tool used. It helps locate the abscess and assess its size and position.
- MRI: Offers better detail than CT, especially in early stages or when abscesses are small or near sensitive brain structures.
3. Blood tests
Elevated white blood cell count and markers of inflammation such as CRP or ESR suggest active infection. Blood cultures help identify the causative organism in systemic cases.
4. Lumbar puncture (with caution)
Doctors generally avoid this when they suspect a brain abscess because of the risk of brain herniation. However, they may use it in rare cases if they rule out an abscess and suspect meningitis instead.
5. Aspiration or biopsy
In some cases, a neurosurgeon may aspirate the abscess using a fine needle guided by CT or MRI. Lab technicians analyse this sample to identify the exact bacteria, fungi, or parasite causing the infection.
In South Africa, urban hospitals with CT and MRI scanners provide better access to evaluations. In rural clinics, referral to a higher-level centre is often necessary, which can delay care.
Diagnosis and Evaluation of Brain Abscess
Accurate and timely diagnosis are critical. Early identification improves outcomes and guides the correct antibiotic or surgical approach.
👉 [Next: Treatment Options for Brain Abscess]