Diagnosis of Bell’s Palsy
Diagnosis of Bell’s palsy is primarily a clinical process, meaning doctors often make the diagnosis based on a person’s symptoms and a physical examination. However, it’s essential to rule out other serious conditions, particularly stroke, which can also cause sudden facial drooping.
Steps in diagnosis typically include:
- Medical history
- The doctor will ask about the onset of symptoms, medical conditions, recent infections, and whether symptoms affect only the face.
- The doctor will ask about the onset of symptoms, medical conditions, recent infections, and whether symptoms affect only the face.
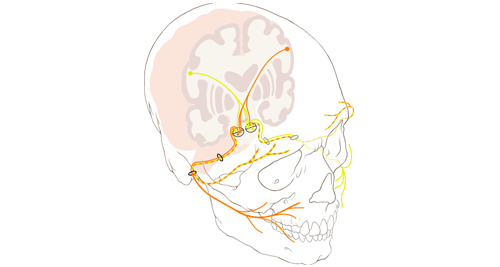
- Physical and neurological exam
- The doctor checks for facial symmetry, strength of facial muscles, eye closure, forehead wrinkling, and smile movement.
- If the forehead can still wrinkle on the affected side, the cause may not be Bell’s palsy (as Bell’s palsy usually affects the whole side of the face).
- Exclusion of other conditions
- Stroke: Often includes limb weakness, slurred speech, or altered consciousness
- Tumour or Lyme disease: May be suspected if symptoms develop slowly or if there is recurrent facial palsy
- Optional tests:
- MRI or CT scan: Ordered if the diagnosis is uncertain, if symptoms progress, or if there are other neurological signs.
- Blood tests: May be done to check for diabetes, HIV, Lyme disease (if exposure is possible), or immune disorders.
- Electromyography (EMG): Measures the electrical activity of muscles and nerve conduction, useful in severe or prolonged cases.
In South Africa, most cases are diagnosed in primary care clinics or emergency units. Public hospitals may provide imaging where needed, especially if red flags like gradual onset or multiple cranial nerve involvement are present.
Diagnosis of Bell’s Palsy
Prompt diagnosis allows early initiation of treatment, which significantly improves recovery rates. Differentiating Bell’s palsy from other conditions, especially stroke, is essential for proper management.
👉 [Next: Treatment of Bell’s Palsy]