Diagnosis of Female Genital Mutilation
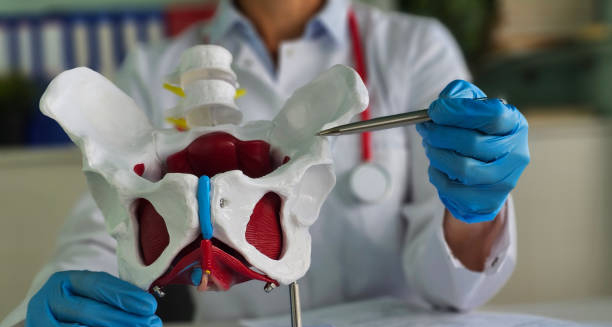
The diagnosis of female genital mutilation is typically made during a clinical examination, especially in contexts where survivors seek care for related complications. Female genital mutilation may also be identified during routine check-ups, maternity care, or when investigating symptoms like chronic pelvic pain or menstrual irregularities.
Clinical Identification
Healthcare professionals may recognise FGM through:
Visual inspection of the external genitalia
Patient disclosure, though many may be hesitant due to fear, stigma, or cultural pressure
Medical history, including past surgeries, childbirth complications, or sexual pain
Complications during gynaecological exams, such as narrow vaginal openings or scarring
In some cases, children or adolescents may be referred by teachers, social workers, or school nurses who observe behavioural or physical signs suggesting they may have undergone FGM or be at risk.
Types of FGM (WHO Classification)
Diagnosing FGM also involves identifying the type:
- Type I: Partial or total removal of the clitoris (clitoridectomy)
- Type II: Removal of the clitoris and labia minora (excision)
- Type III: Narrowing of the vaginal opening by cutting and repositioning the labia (infibulation)
- Type IV: All other harmful procedures (e.g. pricking, burning, scraping)
Understanding the type of FGM is essential for developing appropriate medical and psychological care plans.
Screening in Migrant Populations
In countries with low prevalence of FGM, healthcare systems may screen:
Pregnant women from practising countries
Girls at risk during safeguarding assessments
New arrivals, as part of refugee health services
These screenings are guided by ethical principles and patient consent. They must be done with sensitivity and respect for cultural context.
Legal and Reporting Obligations
In some countries, professionals have a legal duty to report known or suspected cases of FGM, especially in minors. Mandatory reporting laws are intended to protect children at risk but must be balanced with cultural sensitivity and patient trust.
Documentation should:
Use accurate, non-judgemental language
Avoid making assumptions about intent or family dynamics
Focus on the medical findings and any safeguarding concerns
Diagnosis of Female Genital Mutilation
The diagnosis of female genital mutilation is both a medical and social responsibility. Early recognition leads to better care, trauma-informed support, and potentially protects others from harm.
[Next: Treatment and Support for Survivors →]