Diagnosis of ingrown hairs is typically straightforward and based primarily on clinical evaluation. Since ingrown hairs have clear signs—such as raised bumps, local redness, and sometimes visible trapped hairs—doctors can often diagnose them without invasive tests. Still, accurate diagnosis of ingrown hairs matters to rule out other skin problems like acne, folliculitis, cysts, or, in rare cases, skin cancer.
The diagnosis of ingrown hairs usually starts with a detailed medical history. The doctor asks about when the bumps started, how long they have lasted, and any recent hair removal such as shaving, waxing, or tweezing. They also inquire about grooming habits and how often the problem occurs. Knowing if it happens repeatedly or only in certain areas helps guide diagnosis. People who shave often—especially in the beard, underarms, bikini line, or thighs—are more likely to have classic signs of ingrown hairs.
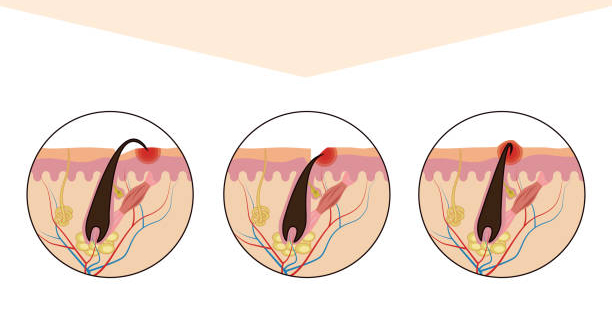
Next comes a physical exam. The doctor checks the affected skin for small red or flesh-coloured bumps or pustules. Sometimes, the hair can be seen curling just below the surface. If pus is present, it may suggest infection, making it important to differentiate from folliculitis. The doctor also feels the area to check for tenderness, warmth, firmness, or cyst-like lumps that may indicate deeper inflammation.
Doctors also consider risk factors during diagnosis of ingrown hairs. Curly or coarse hair increases the chance of hairs bending back into the skin. For example, men of African or Middle Eastern descent often develop pseudofolliculitis barbae, a chronic ingrown hair condition affecting the beard. Knowing these details helps confirm the diagnosis and plan prevention.
Diagnosis of Ingrown Hairs
In some cases with deep cysts or persistent inflammation, dermoscopy may be used. This handheld device magnifies and lights the skin to reveal embedded hairs, follicle damage, or pigment changes not seen by the naked eye. Dermoscopy also helps distinguish ingrown hairs from other conditions like basal cell carcinoma or nodular acne.
If infection is suspected—marked by discharge, severe redness, fever, or swollen lymph nodes—a bacterial culture may be taken. Swabbing the lesion identifies the bacteria causing infection, often Staphylococcus aureus. Sometimes antibiotic sensitivity testing is needed to select the right medication.
When diagnosis is unclear or symptoms persist despite treatment, doctors check for other conditions that mimic ingrown hairs. These include:
- Folliculitis: infection or irritation of hair follicles
- Acne vulgaris: pimples and cysts common in oily skin
- Hidradenitis suppurativa: chronic lumps and abscesses in sweat gland areas
- Keratosis pilaris: rough, small bumps from excess keratin
- Epidermoid cysts: benign lumps without hair or typical inflammation
In rare or stubborn cases, a skin biopsy may be done. This removes a small skin sample under local anaesthetic for lab examination. Biopsy confirms trapped hairs, chronic inflammation, or excludes serious diseases. However, most ingrown hair cases do not require biopsy.
Doctors may also investigate hormonal or systemic causes during diagnosis of ingrown hairs. Blood tests check androgen levels, thyroid function, or insulin resistance, especially in women with excessive hair growth linked to conditions like PCOS. Addressing these factors helps manage hair growth and reduce ingrown hairs.
Patients experiencing distress from ingrown hairs may benefit from mental health support. Anxiety, obsessive picking, or self-harm can worsen skin damage. Referral to a psychologist or psychodermatologist can be part of holistic care.
In summary, diagnosis of ingrown hairs mainly relies on medical history and physical exam. For difficult cases, dermoscopy, bacterial cultures, or biopsy may be needed. Recognizing risk factors like hair type, grooming, and hormones allows better treatment and prevention. Accurate diagnosis prevents complications such as infection, scarring, and pigmentation changes.