The diagnosis of ingrown toenail is primarily a clinical one, made through physical examination and patient history rather than complex laboratory tests or imaging. While the condition may seem simple, early and accurate diagnosis is essential. It helps determine the severity, spot complications, and choose the best treatment. Quick action can stop the problem from getting worse, especially in people with diabetes or circulation problems.
Diagnosis usually starts with a conversation about the patient’s symptoms and medical background. Most people report pain, tenderness, redness, or swelling on one side of the toenail—usually on the big toe. The discomfort may begin mildly and grow worse over time. Activities like walking, standing, or wearing shoes often make the pain sharper. One common sign is pain that increases when applying pressure, like when putting on socks or shoes.
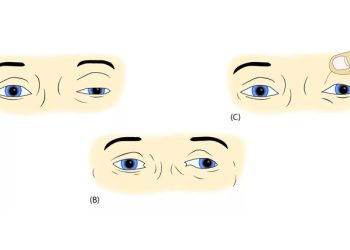
Next, a healthcare provider—often a general practitioner or podiatrist—will examine the toe. Early signs include mild redness or swelling where the nail presses into the skin. In more severe cases, the nail edge breaks through the skin. There may be pus, drainage, or red, swollen tissue. The skin might look shiny or feel warm.
If the ingrown toenail is infected, symptoms will go beyond pain and redness. You may see yellow or green discharge, a bad smell, or extreme tenderness. The area may feel hot to the touch. At this stage, the diagnosis of ingrown toenail must also check if the infection has spread. Infections that move beyond the nail fold can cause serious issues like cellulitis or abscesses.
Doctors also look for granulation tissue—red, soft skin that grows as the body tries to heal. This tissue can bleed easily and may cover part of the nail. While it signals healing, it can also trap the nail further and make things worse.
Sometimes, other conditions can mimic the symptoms. Doctors use a differential diagnosis to rule out problems like fungal infections, paronychia, subungual haematomas, or nail tumours. These conditions can also cause pain or nail changes but follow different patterns. If the diagnosis isn’t clear, doctors may take a tissue sample or do a culture—especially if infection or cancer is suspected.
The diagnosis of ingrown toenail requires extra care in patients with diabetes, poor circulation, or nerve damage. These people may not feel typical warning signs like pain. What looks like a minor issue could already be a serious infection. During the exam, doctors may check nerve response with a monofilament and look at skin health. They may also test blood sugar and circulation if needed.
In rare cases, X-rays may be helpful. For example, if swelling makes it hard to see the nail or if the doctor suspects infection in the bone. These images can show whether the infection has spread or if something else, like a foreign object, is causing the problem.
For people who keep getting ingrown toenails, diagnosis includes checking for foot shape problems like flat feet, bunions, or unusual walking patterns. These issues can increase pressure on the toes. Doctors will also review shoe choices and grooming habits. Identifying the root cause is key to stopping future flare-ups.
Nail care habits matter too. Trimming nails too short or rounding the corners often leads to trouble. During the diagnosis of ingrown toenail, doctors ask about nail cutting methods, footwear, hygiene, and past injuries. This is also a chance to teach patients better habits to avoid future issues.
Documenting the findings is an important part of diagnosis. It helps track the stage of the problem—mild, moderate, or severe. This guides treatment. Mild cases might just need foot soaking and better shoes. Moderate ones may need partial nail removal and antibiotics. Severe or frequent cases often call for nail surgery, possibly with a chemical to stop regrowth.
In summary, the diagnosis of ingrown toenail is a clear but vital step. A detailed exam and patient history reveal the problem and its cause. Early and accurate diagnosis helps avoid infection, pain, and repeat problems. Doctors must be especially careful with people who have other health issues. With prompt diagnosis, patients can get relief, heal properly, and protect their feet long-term.