Diagnosis of Legionnaires’ disease is a crucial step in preventing severe complications and ensuring timely medical intervention.
The key to effective treatment lies in spotting the illness early. This is important because it often looks like other types of pneumonia or flu. Quick diagnosis of Legionnaires’ disease can lower the risk of serious issues like breathing failure, blood infections, and even death. This is especially true for older adults or people with weak immune systems.
Doctors often see symptoms that resemble other lung infections, especially in the early stages. Because of this, they must use a mix of checking symptoms, asking about the patient’s past, and running special lab tests. The first thing a doctor usually does is ask questions about recent activities. These may include recent hotel stays, hospital visits, use of hot tubs, or work in large buildings with air-conditioning or water systems. These places are often where Legionella bacteria grow—the bacteria that causes the illness.
First Steps in Diagnosis of Legionnaires’ Disease
Next comes a physical check-up. Doctors will listen to the lungs, check body temperature, measure oxygen levels, and see how hard the patient is breathing. These signs alone don’t give a final answer, but they help doctors decide which tests to run. Symptoms like fever, coughing, trouble breathing, and signs like diarrhoea or confusion often raise concerns. These red flags push the doctor to check for Legionnaires’ disease more carefully.
The most trusted test is the urinary antigen test. It checks for signs of Legionella pneumophila serogroup 1 in urine. This test works fast and gives accurate results, often within hours. It helps a lot in urgent care settings. This is useful because the bacteria may die before they can be cultured in a lab.
But this test does have a drawback. It only checks for one type of Legionella. This type is the most common, but it’s not the only one. So, if symptoms are strong and the test is negative, doctors should dig deeper. In these cases, a sputum culture becomes useful. Doctors collect a sample of mucus from the lungs and grow it on special material called BCYE agar. This process helps find the exact type of bacteria and test which medicines work best. But it takes a few days to get the results.
Advanced Testing for Diagnosis of Legionnaires’ Disease
Another powerful tool is PCR (polymerase chain reaction). This test looks for Legionella DNA in lung fluids like mucus or fluid taken from deep in the lungs. It gives quick results and finds more than one type of Legionella. Because of this, it gives better coverage than the urine test.
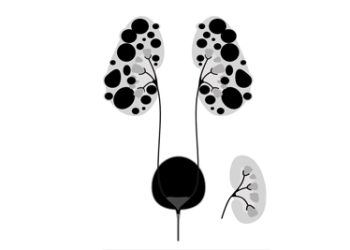
In hospitals, especially for very sick patients, doctors may order X-rays or CT scans. These pictures help show how much of the lung is infected. They also show if there is extra fluid or other issues. But these images look the same as other types of pneumonia, so they can’t confirm the diagnosis alone. Still, they help guide the rest of the testing.
Blood tests offer more clues. Doctors often see high white blood cell counts, low sodium levels, high liver enzymes, and signs of inflammation like raised CRP or ESR levels. These clues aren’t specific to Legionnaires’ disease but help confirm that something serious is happening. That pushes doctors to do more targeted testing.
Sometimes doctors perform a bronchoscopy. They gently place a thin tube into the lungs to collect samples. This is usually done when the disease is very severe or when the patient can’t cough up mucus. The samples are then sent for PCR, culture, or cell testing.
Broader Tools and Public Health
For big outbreaks or to gather public health data, doctors may run blood tests to check for Legionella antibodies. This kind of testing takes weeks and isn’t helpful right away. It’s more useful for checking exposure in past cases or understanding patterns in groups of people.
Doctors should think about the diagnosis of Legionnaires’ disease when a person with pneumonia doesn’t get better after using common antibiotics like penicillin or cephalosporins. Legionella doesn’t respond to these medicines. If there’s no improvement after two or three days, this may be a sign that a different test and treatment are needed.
Correct diagnosis helps the patient but also protects the public. Once doctors confirm a case, health officials may step in. They often check places like hotels, hospitals, or factories to test the water systems. Finding the source can stop others from getting sick. So, catching the illness early protects both the person and the community.
Improving Detection and Recovery
Another problem is that many cases of Legionnaires’ disease go undiagnosed. The symptoms can look like many other illnesses. Often, doctors don’t test for it unless they strongly suspect it. Some people may even get treated for something else by mistake. That’s why it’s vital for doctors to stay alert, especially during certain seasons or in areas where the risk is higher.
Patients who recover from the illness often need follow-up visits. Doctors may do lung tests or take new X-rays to check healing. If diagnosis is delayed, healing may take longer and the risk of problems increases. This shows why early and correct testing is so important.
To sum up, the diagnosis of Legionnaires’ disease depends on patient history, check-ups, images, and special lab tests. Finding it early helps people get better faster and can stop new cases from starting. With more people travelling, living in cities, and using shared water systems, doctors must stay aware and use every tool they have to fight this often missed but serious illness.