Diagnosis of liver cancer involves a multi-step process that integrates clinical assessment, imaging studies, laboratory tests, and, in some cases, tissue sampling.
Since early signs are often unclear or missing, many people are diagnosed late. That’s why it’s so important to find liver cancer early, especially in people with high risk like hepatitis, cirrhosis, or other liver problems. A strong understanding of the diagnosis of liver cancer helps doctors catch it early, choose the best treatment, and predict outcomes.
Medical History, Symptoms, and First Steps
Doctors begin by asking about the patient’s medical history and performing a full exam. They look for risk factors like long-term hepatitis B or C, heavy alcohol use, family history of liver problems, or exposure to toxins like aflatoxins. They also ask about symptoms such as unexplained weight loss, tiredness, pain on the right side of the belly, or yellowing of the skin.
During the physical exam, doctors check for signs like an enlarged liver (hepatomegaly), fluid buildup in the belly (ascites), or jaundice. These findings can point toward possible liver cancer and lead to more testing.
Imaging Studies in Diagnosis of Liver Cancer
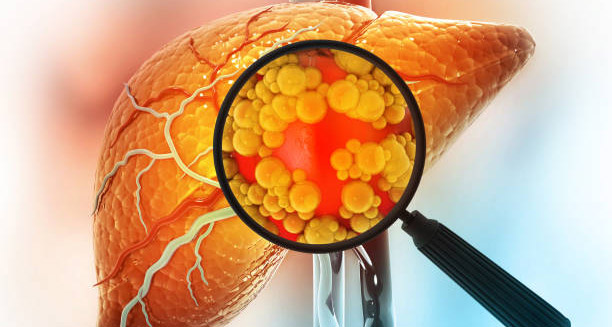
If doctors suspect liver cancer, the next step is usually imaging. Ultrasound is often the first test. It’s simple, safe, cheap, and available in most places. In high-risk patients, doctors often use ultrasound regularly to spot tumours early.
If ultrasound shows something unusual, more detailed scans are done. A CT scan or MRI with contrast gives a clearer view of the liver. These tests help doctors see how many tumours are present, how big they are, and where they are located. A typical sign of liver cancer on these images is a bright spot during the arterial phase and fading in the venous phase. This pattern, along with cirrhosis, can strongly suggest hepatocellular carcinoma (HCC).
Blood Tests, Biomarkers, and the Role of Biopsy
Blood tests also play a key part in the diagnosis of liver cancer. The main marker is alpha-fetoprotein (AFP), which often rises in people with HCC. However, AFP isn’t perfect. Some liver cancers don’t produce it, and other liver issues can cause AFP to rise too. Still, when AFP levels are used alongside imaging, they can help confirm the diagnosis.
Other markers like des-gamma-carboxy prothrombin (DCP) and AFP-L3 can also help. At the same time, liver function tests — like bilirubin, albumin, liver enzymes, and clotting time — help doctors understand how well the liver is working. This is important for choosing treatment.
In some cases, imaging and blood tests don’t give a clear answer. When this happens, a biopsy may be needed. Doctors use a needle to take a small sample of liver tissue, often guided by ultrasound or CT scan. A pathologist checks this sample under a microscope to see if cancer cells are present.
But biopsies do carry some risk. Liver tumours have many blood vessels, so there’s a small chance of bleeding. There’s also a rare chance of cancer spreading along the needle path. That’s why doctors only do biopsies when needed.
Staging Systems and Transplant Considerations
Once doctors confirm liver cancer, they must figure out its stage. Staging shows how far the cancer has spread and helps guide treatment choices. The Barcelona Clinic Liver Cancer (BCLC) system is one of the most used. It looks at tumour size and number, liver function (Child-Pugh score), physical condition, and symptoms to suggest treatment plans.
Another system, called TNM staging, focuses on tumour size (T), lymph node spread (N), and distant spread (M). This system helps in planning surgery. Doctors may also scan the chest or bones to check for cancer spread. In some cases, they use PET scans to find cancer outside the liver.
For patients who may get a liver transplant, doctors also check if they meet the Milan criteria. This includes one tumour ≤5 cm or up to three tumours each ≤3 cm, with no blood vessel invasion or spread outside the liver. Meeting these rules means a transplant could be an option.
Surveillance, AI Tools, and the Future of Diagnosis of Liver Cancer
Surveillance is a critical part of the diagnosis of liver cancer, especially for people with cirrhosis or chronic hepatitis B. Doctors recommend an ultrasound every six months, with or without AFP testing. This allows them to catch liver cancer early, when treatments like surgery, ablation, or transplant can still cure it.
New technologies are also shaping the future. Artificial intelligence (AI) and radiomics can look at scans in much more detail than the human eye. These tools may soon help doctors find liver cancer earlier or predict how it will behave. At the same time, liquid biopsies — tests that find tumour DNA or RNA in the blood — are being tested for early, non-invasive detection.
Final Thoughts on Diagnosis of Liver Cancer
To sum up, the diagnosis of liver cancer includes history taking, imaging, blood tests, and sometimes biopsy. Catching liver cancer early gives patients the best chance for survival. For people at risk, regular screening is essential. As technology improves, better tests and smarter tools will help detect this aggressive cancer sooner and more accurately.