Diagnosing low testosterone requires a careful mix of medical history, physical exam, and lab testing. Testosterone levels naturally vary throughout the day and can be influenced by many factors, so one low test result isn’t enough to confirm deficiency. A thorough, evidence-based approach helps distinguish true low testosterone from temporary dips caused by stress, illness, or medications.
The goal is to match symptoms with hormone test results. This ensures only men who need treatment receive it, avoiding unnecessary hormone therapy in those with normal hormone variation.
1. Initial Clinical Evaluation
Diagnosis begins with a detailed consultation between patient and healthcare provider. The clinician asks about:
- Symptoms: Fatigue, low libido, erectile dysfunction, depression, muscle loss, and other signs of low testosterone.
- Medical history: Chronic diseases (diabetes, sleep apnoea), testicular injury or surgery, past chemotherapy, radiation, or steroid use.
- Medications: Drugs like opioids, corticosteroids, and some antidepressants can lower testosterone.
- Lifestyle: Sleep habits, stress, exercise, alcohol, and smoking affect hormone balance.
- Fertility concerns: Difficulty conceiving may lead to hormonal testing as part of infertility evaluation.
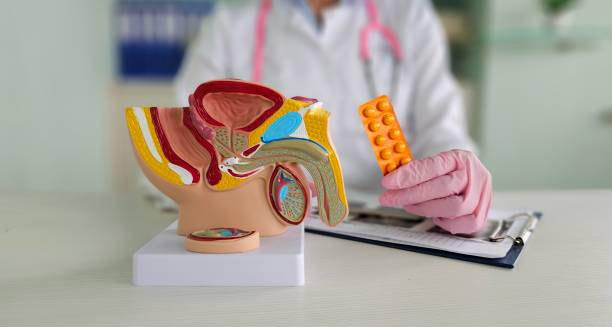
A physical exam checks for:
- Small or soft testes
- Reduced body or facial hair
- Increased belly fat
- Breast enlargement (gynecomastia)
- Reduced muscle bulk and strength
These findings help confirm suspicion and guide lab testing.
2. Laboratory Testing
Blood tests measure serum testosterone to confirm deficiency.
a) Total Testosterone Test
- Test in early morning (7–10 a.m.) when levels peak.
- Repeat testing on a different morning if the first is low, due to natural fluctuations.
- Reference ranges:
- < 8 nmol/L (230 ng/dL): Deficiency confirmed
- 8–12 nmol/L (230–350 ng/dL): Borderline; needs further evaluation
- 12 nmol/L (350 ng/dL): Usually normal
b) Free Testosterone Test
- Total testosterone includes bound and free hormone; only free testosterone is active.
- Ordered if total testosterone is borderline or symptoms don’t match results.
- Calculated from total testosterone, SHBG, and albumin levels.
c) LH and FSH
- These pituitary hormones regulate testicular function.
- High LH/FSH + low testosterone suggests primary testicular failure.
- Low/normal LH/FSH + low testosterone suggests secondary (pituitary or hypothalamic) hypogonadism.
d) Prolactin Levels
- High prolactin can suppress LH/FSH, lowering testosterone.
- Elevated prolactin may indicate a pituitary tumor and require imaging.
e) SHBG
- Binds testosterone in blood.
- Abnormal SHBG levels affect free testosterone availability.
- Testing helps interpret borderline results.
3. Imaging Studies (If Needed)
Imaging is not routine but may be done when indicated:
- Pituitary MRI: For suspected secondary hypogonadism with low LH/FSH, high prolactin, headaches, or vision changes.
- Scrotal ultrasound: To check testicular size, structure, or masses if exam is abnormal.
- Bone density scan (DEXA): To assess bone loss in men with long-standing low testosterone.
4. Other Blood Tests and Assessments
Additional tests may clarify overall health or treatment readiness:
- Complete blood count (CBC): To check for anaemia caused by testosterone deficiency.
- Liver and kidney function tests: To exclude other systemic illnesses.
- Lipid and glucose profiles: Because metabolic syndrome, diabetes, and cholesterol issues often coexist with low testosterone.
5. Confirming the Diagnosis
Low testosterone diagnosis requires both symptoms and lab evidence. Guidelines advise against treating based on blood tests alone.
- Men with testosterone <8 nmol/L and classic symptoms usually qualify for diagnosis and treatment.
- Borderline levels (8–12 nmol/L) require case-by-case assessment, repeat tests, and free testosterone measurement.
- Asymptomatic men with low levels generally should not be treated.
6. Excluding Temporary Causes
Before confirming low testosterone, rule out temporary factors that can lower hormone levels:
- Acute illness or infection
- Sleep deprivation
- Overtraining or sudden weight loss
- Recent steroid or medication use that suppress hormone production
Retest after these issues resolve to avoid misdiagnosis.
In conclusion, diagnosing low testosterone is a detailed process that matches symptoms with repeated, accurate hormone testing. This precision avoids unnecessary treatment or missed diagnosis. Proper diagnosis is the first step to restoring hormone balance and improving long-term quality of life.