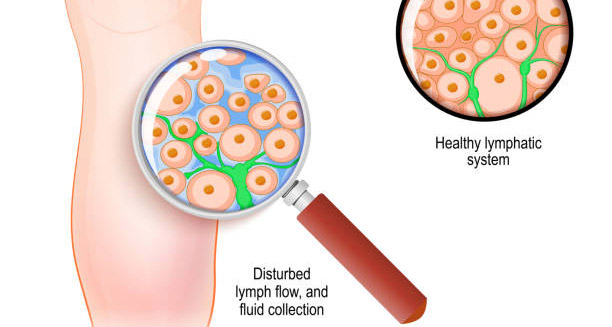
Diagnosis of lymphoedema is a clinical process that involves evaluating a patient’s symptoms, physical appearance, medical history, and risk factors. Because the condition shares similarities with other types of swelling (such as venous insufficiency, deep vein thrombosis, or lipedema), it’s vital to make a precise diagnosis to ensure appropriate treatment. Early and accurate diagnosis of lymphoedema can significantly improve quality of life and reduce the risk of complications.
Clinical History and Physical Examination
Diagnosis of lymphoedema usually starts with a full medical history and physical exam. The healthcare provider will ask about:
- When the swelling started and how long it’s lasted
- Any past surgery, cancer treatment, or radiation
- Recent infections or injuries
- Family history of lymph or vein problems
- Whether the swelling gets worse during the day
- Any past skin infections or cellulitis
During the exam, the doctor looks for signs such as:
- Swelling that affects one limb more than the other
- Soft, pitting swelling in early stages
- Hard, thick skin in later stages
- Skin folds or thick patches
- A positive Stemmer’s sign — when the skin at the base of the toe or finger cannot be pinched
These findings help guide the next steps.
Ruling Out Other Causes
Before confirming lymphoedema, doctors need to rule out other possible reasons for the swelling. Conditions that look similar include:
- Deep vein clots (DVT)
- Poor blood flow in the veins
- Heart failure
- Kidney or liver problems
- Infections like cellulitis
- Lipedema (fat build-up, often in both legs but not the feet)
Tests such as blood work, urine tests, and vein scans using Doppler ultrasound help exclude other causes.
Imaging Tests in the Diagnosis of Lymphoedema
When a physical exam doesn’t give clear answers, imaging tests help confirm diagnosis of lymphoedema. These tests show if there are problems with the lymph system.
a) Lymphoscintigraphy
This is the most trusted test for checking lymph flow. A small amount of dye is injected under the skin. A special camera tracks how the dye moves through the lymph vessels. This test can show blocked vessels or missing lymph nodes.
b) Ultrasound
Doppler ultrasound helps rule out blood clots or vein issues. Although it doesn’t show the lymph system itself, it’s helpful in excluding other problems and may show thick tissue in swollen areas.
c) MRI or CT Scan
Doctors use these scans to look at soft tissues and check for fluid, fibrotic tissue, or tumours pressing on lymph vessels.
d) Indocyanine Green (ICG) Lymphography
This newer test uses a glowing dye and a special camera to see lymph vessels near the skin. It gives detailed images and helps plan surgery when needed.
Bioimpedance Spectroscopy
This non-invasive test checks how well tissues resist electrical current. Fluid changes how the current moves, so the test can detect swelling early — even before it’s visible.
Doctors often use it in cancer clinics to monitor patients at risk. It’s especially useful in detecting early lymphoedema in breast cancer survivors.
Limb Volume Measurement
Measuring limb size helps track swelling and monitor progress over time. Doctors may use:
- A tape measure at standard points
- Water displacement to measure volume
- Perometry, which uses light beams to calculate limb size
These measurements support both diagnosis and treatment planning.
Primary vs Secondary Lymphoedema
Once lymphoedema is confirmed, it’s important to find out if it’s primary (from birth or inherited) or secondary (caused by something else).
Doctors may diagnose primary lymphoedema when:
- There’s no history of surgery, injury, or cancer
- Family members have similar symptoms
- Swelling started young, such as in childhood or early adulthood
Secondary lymphoedema is more common and linked to:
- Surgery or radiation therapy
- Repeated infections
- Cancer blocking the lymph flow
In rare cases, genetic tests can help diagnose primary lymphoedema, especially when there are other unusual features.
Referral to a Specialist
Because the condition is complex, many patients need to see a lymphoedema or vascular specialist. These experts can read imaging results, assess risks, and create a treatment plan.
A full team approach often includes physiotherapists, skin specialists, and oncology professionals. Working together gives patients the best care.
Summary
The diagnosis of lymphoedema uses a careful mix of history, physical exams, and imaging tests. Ruling out other causes is essential. Early diagnosis helps prevent swelling from getting worse and lowers the risk of infection or hard tissue build-up.
With a proper diagnosis, patients can start a care plan that improves comfort, function, and daily life.