Early and accurate identification of the diagnosis of lymphoma is crucial for determining the most appropriate treatment strategy and improving long-term outcomes.
Diagnosing lymphoma can be tricky. It often looks like infections, autoimmune diseases, or other cancers that cause similar symptoms. Since lymphoma can appear almost anywhere in the body and includes over 70 types, doctors follow a clear step-by-step approach.
Clinical Evaluation and Imaging
Doctors begin the diagnosis of lymphoma with a detailed clinical evaluation. They ask about symptoms like unexplained weight loss, constant tiredness, fever, night sweats, or swollen lymph nodes. Then, they carefully check the body for swollen nodes in the neck, armpits, or groin. They also look for signs of organ swelling or skin changes.
If lymphoma seems likely, doctors order imaging tests to find the location and spread of the disease. These tests include:
- Chest X-ray: Finds enlarged lymph nodes in the chest area.
- Ultrasound: Checks lymph nodes and organs in the abdomen.
- CT scan: Gives detailed pictures of lymph nodes and organs to check spread.
- PET scan: Often combined with CT, it highlights active cancer by showing areas with high metabolism.
- MRI: Best for checking brain or spinal cord involvement.
Even though imaging helps locate lymphoma, it cannot confirm the diagnosis.
Biopsy and Laboratory Testing
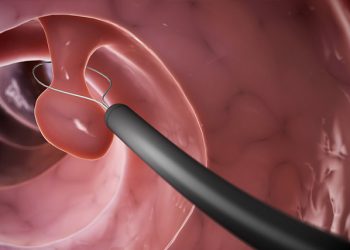
Doctors need to remove tissue for a definite diagnosis. Usually, they perform a lymph node biopsy. The best method is an excisional biopsy, which removes the whole lymph node. This gives enough tissue to study. If this is not possible, a core needle biopsy removes part of the node, but it may be less clear.
A pathologist studies the tissue under a microscope. They look at cell size, shape, and arrangement. This helps tell apart Hodgkin lymphoma, which has special Reed-Sternberg cells, from non-Hodgkin lymphoma, which does not.
Doctors also use immunophenotyping tests like flow cytometry or immunohistochemistry. These tests identify markers on the surface of cancer cells, such as CD20 on B-cell lymphomas or CD3 on T-cell lymphomas. These details help classify the lymphoma subtype and guide treatment.
Genetic and Molecular Tests
Genetic tests check for changes like translocations or mutations in lymphoma cells. For example, the t(14;18) translocation is common in follicular lymphoma, and t(11;14) appears in mantle cell lymphoma. Tests such as FISH (fluorescence in situ hybridisation) and PCR (polymerase chain reaction) detect these changes accurately.
Blood tests also play a key role. These include:
- Full blood count to find anemia or low blood cells
- LDH levels to show cell breakdown, often higher in aggressive lymphomas
- Inflammation markers like ESR and CRP
- Liver and kidney tests to check organ health
- Tests for HIV and hepatitis B or C, since infections can affect treatment choices
Sometimes, doctors take a bone marrow sample if they suspect the disease has spread there. This involves drawing marrow from the pelvic bone to assess the cancer’s reach.
If lymphoma might involve the brain or spinal cord, especially in aggressive forms or when neurological signs appear, doctors perform a lumbar puncture (spinal tap).
Staging and Multidisciplinary Review
After gathering all the information, doctors stage the lymphoma using the Ann Arbor Staging System. This system helps show if the disease is localised or widespread and notes the presence of B symptoms (fever, weight loss, night sweats):
- Stage I: One lymph node area or a single organ
- Stage II: Two or more lymph node areas on the same side of the diaphragm
- Stage III: Lymph nodes on both sides of the diaphragm
- Stage IV: Spread to one or more organs outside the lymphatic system
Each stage gets an “A” if no B symptoms are present or “B” if they are.
Finally, a team of specialists—haematologists, oncologists, pathologists, and radiologists—reviews the case. They confirm the diagnosis of lymphoma and plan the best treatment based on type, stage, and patient health.
Summary: The Role of Early Diagnosis in Managing Complications of Lymphoma
The diagnosis of lymphoma requires careful steps: clinical checks, imaging, biopsy, lab tests, and staging. Early and accurate diagnosis leads to better treatment and improved outcomes. It also helps doctors anticipate and manage complications of lymphoma during treatment. With new diagnostic tools and genetic profiling, doctors can identify even rare lymphoma types and personalise care. This progress marks a new era in fighting lymphoma and its complications.