Diagnosis of Marfan Syndrome
The Diagnosis of Marfan Syndrome is a complex process that integrates physical examination, family history, specialised imaging, and sometimes genetic testing. Due to its variable presentation and overlapping features with other connective tissue disorders, reaching an accurate Diagnosis of Marfan Syndrome requires a careful, multidisciplinary approach. While some cases are evident early in life due to striking physical features, others go undiagnosed until adulthood, especially when cardiovascular or ocular symptoms develop. Early diagnosis can be life-saving, as it enables proactive monitoring and management of potentially fatal complications such as aortic dissection.
The Ghent Criteria: A clinical gold standard
Doctors use the internationally accepted Ghent Nosology to guide diagnosis. Updated in 2010, it highlights two main features:
- Aortic root aneurysm or dissection
- Ectopia lentis (lens dislocation)
If either of these is found, and genetic testing or body signs also suggest Marfan syndrome, the diagnosis is supported. When a family history exists, doctors may lower the diagnostic threshold slightly. This is because Marfan syndrome often runs in families.
First steps in clinical evaluation
The first step in the Diagnosis of Marfan Syndrome involves a full check-up by a skilled doctor. This check-up includes several important parts:
- Body measurements: Doctors look at height, arm span (often longer than height), body segment ratio, and hand or finger shape.
- Skeletal check: They look for chest shape issues, spine curves, flat feet, high-arched palate, loose joints, and specific facial traits.
- Eye check: An eye exam checks vision and looks for lens shift, nearsightedness, or other vision problems.
- Heart check: The doctor listens for heart murmurs that could point to valve problems.
If many of these signs appear, more tests and genetic reviews often follow.
Imaging studies: visualising structural changes
Scans and images are key in confirming the Diagnosis of Marfan Syndrome. They help spot serious issues inside the body, even when no symptoms are present.
1. Echocardiography
This heart scan is very important:
- It measures the size of the aortic root and ascending aorta.
- It spots valve problems like prolapse or leaking.
- It helps track changes in the aorta over time.
2. MRI or CT angiography
These scans help when:
- The echo images aren’t clear.
- A full view of the entire aorta is needed.
- Doctors need details before heart surgery.
3. Spine imaging
An MRI of the lower spine can show dural ectasia. This is when the fluid sac around the spine becomes wider—a common but silent sign of Marfan syndrome.
4. Eye imaging
Doctors may use OCT or ultrasound scans to check for lens shift. They also check the back of the eye for signs of damage or retinal problems.
Genetic testing and counselling
Genetic tests now play a big role, especially when:
- Physical signs are unclear or mild.
- A child is being checked before clear signs show up.
- Family members of someone with Marfan syndrome are being tested.
Important notes:
- Marfan syndrome comes from a problem in the FBN1 gene. This gene makes fibrillin-1, which helps keep body tissues stretchy and strong.
- A harmful change in this gene strongly supports the Diagnosis of Marfan Syndrome, especially when paired with aorta or eye issues.
- Genetic testing can also tell Marfan apart from similar conditions like Loeys-Dietz syndrome, Ehlers-Danlos syndrome, or MASS phenotype.
Even though it’s not always needed, this test gives useful details for family planning and risk checks.
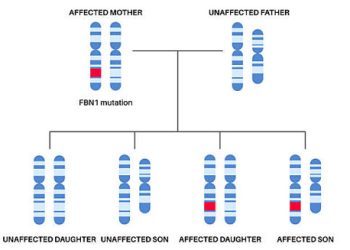
Family history: a critical component
Marfan syndrome passes from parent to child. If one parent has it, each child has a 50% chance of getting it.
Because of this:
- Doctors always ask about family health—heart problems, sudden deaths, tall height, or past diagnoses.
- Close family members often get screened with heart and eye tests.
- If a harmful gene change is found in the first patient, doctors can test family members quickly, without waiting for symptoms.
Systemic score: evaluating multi-system signs
The updated Ghent criteria include a systemic score. This helps count how many body signs point to Marfan syndrome.
Points go to signs like:
- Thumb and wrist signs (flexible joints)
- Chest shape issues
- Spine curves
- Elbow that doesn’t fully straighten
- Facial traits
- Nearsightedness
- Flat feet
- Stretch marks
- Collapsed lung
- Dural ectasia
If someone scores 7 or more, and other signs are also present, doctors strongly suspect Marfan syndrome. This scoring helps when signs are borderline, especially in young people.
Differential diagnosis: ruling out similar conditions
Many conditions look like Marfan syndrome, so doctors must rule them out:
| Condition | Key Feature |
|---|---|
| Loeys-Dietz Syndrome | Twisted arteries, wide-set eyes, cleft palate, fast-growing aneurysms |
| Ehlers-Danlos Syndrome | Very stretchy skin, weak tissues, no aorta enlargement |
| Homocystinuria | Intellectual issues, blood clots, lens shift downward |
| MASS phenotype | Similar signs but no aorta or eye problems |
| Stickler Syndrome | Severe nearsightedness, eye damage, hearing loss, flat face |
Ruling out these helps because their treatments and risks differ from Marfan syndrome.
When to suspect Marfan syndrome
Doctors should think about the Diagnosis of Marfan Syndrome when these signs appear:
- A tall, thin person with long arms or fingers
- Sunken or bulging chest
- A new heart murmur in a young person
- Strong or worsening nearsightedness
- Sudden lens shift
- Family history of sudden heart death or tissue disorder
- Curved spine or loose joints without clear reason
- Collapsed lung in a tall, slim person
General doctors, children’s doctors, eye doctors, and bone specialists must stay alert to these signs and refer when needed.
Importance of early diagnosis
Catching the Diagnosis of Marfan Syndrome early allows:
- Regular checks of the aorta and heart valves
- Safer daily habits
- Early surgery when needed
- Saving eyesight through checks and fixes
- A full team of doctors to manage care
Without diagnosis, people face a high risk of sudden death from a burst aorta. With early help and modern care, people with Marfan syndrome can live long, active lives.
Summary: Diagnosis of Marfan Syndrome in a modern clinical setting
The Diagnosis of Marfan Syndrome includes a full exam, imaging, systemic scoring, gene testing, and family checks. Doctors use the Ghent criteria to pull all these together. Signs like aorta enlargement, lens shift, flexible joints, body shape, and gene changes confirm the diagnosis. Finding it early saves lives and improves health for years to come.