Giant Cell Arteritis
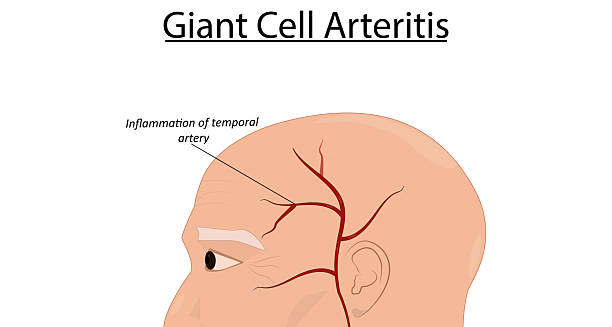
Giant cell arteritis is a serious inflammatory condition that affects the blood vessels, particularly the large and medium-sized arteries of the head and neck. Also known as temporal arteritis, giant cell arteritis occurs when the immune system mistakenly attacks the artery walls, leading to inflammation, swelling, and damage to the vessel lining. This condition most commonly involves the temporal arteries, which run along the sides of the head, but it can affect other arteries as well, including the aorta.
The most significant danger of untreated giant cell arteritis is sudden vision loss, which can occur if the arteries supplying the eyes become inflamed or blocked. Prompt diagnosis and treatment are essential to prevent irreversible complications. The condition predominantly affects individuals over the age of 50 and is more common in women than in men.
Despite its name, giant cell arteritis does not refer to a physically enlarged artery but rather to the giant cells—a type of immune cell—seen under the microscope in biopsied tissue. These cells contribute to the aggressive inflammation that characterises the disease.
Who Is Affected?
Giant cell arteritis primarily affects:
People over the age of 50, with incidence increasing with age
Women, who are two to three times more likely than men to develop it
Individuals of Northern European descent, though it can occur in any ethnic group
People with a history of polymyalgia rheumatica (PMR)—an inflammatory disorder that frequently coexists with giant cell arteritis
PMR and GCA are thought to be related inflammatory diseases, with up to 50% of patients with one developing symptoms of the other.
Key Features and Impact
Giant cell arteritis can present with a range of symptoms that may develop suddenly or gradually. The inflammation causes narrowing or blockage of affected arteries, which can severely reduce blood flow and oxygen supply to key organs and tissues.
In the short term, the condition can cause:
Severe headaches
Jaw pain when chewing
Scalp tenderness
Double vision or sudden blindness
In the long term, if untreated, it may lead to:
Permanent vision loss
Aneurysm formation, particularly in the aorta
Stroke, if arteries supplying the brain are affected
Because of the potentially devastating consequences, early identification and treatment are vital.
How It Develops
The exact cause of giant cell arteritis is not fully understood, but it is believed to be an autoimmune reaction—a condition in which the body’s immune system attacks its own tissues. In GCA, immune cells mistakenly target the lining of arteries, particularly those with elastic components like the temporal artery.
This immune attack causes inflammation and the formation of granulomas, which often contain multinucleated giant cells—hence the name. These granulomas thicken the arterial walls, narrow the lumen (internal space), and reduce or block blood flow.
Is It Common?
Giant cell arteritis is the most common form of systemic vasculitis in adults over 50. Its prevalence varies by region and ethnicity, with higher rates reported in Scandinavian and North American populations.
In the UK and many parts of Europe, the estimated annual incidence is around 15 to 30 cases per 100,000 people over age 50.
Early Symptoms to Watch For
Symptoms of GCA can overlap with many other conditions, making diagnosis a challenge. The most common early signs include:
New-onset headaches, especially around the temples
Tender scalp, making it painful to brush hair or wear a hat
Jaw claudication—pain or fatigue in the jaw muscles while chewing
Vision changes, such as blurred or double vision
General fatigue, low-grade fever, and unintended weight loss
Pain and stiffness in the shoulders or hips, suggesting coexisting PMR
Some individuals may have subtle or vague symptoms, such as general malaise, which delays diagnosis.
Why Vision Loss Happens
One of the most feared complications of giant cell arteritis is permanent vision loss, which occurs in up to 20% of untreated cases. This usually happens when inflammation affects the posterior ciliary arteries that supply the optic nerve. Reduced blood flow leads to ischaemia (oxygen deprivation) and irreversible optic nerve damage.
Visual symptoms may include:
Sudden, painless loss of vision in one eye
Transient blurred vision or episodes of visual blackouts (amaurosis fugax)
Double vision due to muscle involvement
Immediate medical intervention can sometimes save vision in the other eye, but damage to the first is usually irreversible if treatment is delayed.
Diagnosis and Outlook
Early diagnosis and treatment with high-dose corticosteroids can dramatically reduce the risk of complications. Once inflammation is controlled, medication is tapered over time, but careful monitoring is required to prevent relapse.
Modern treatment approaches also include the use of steroid-sparing agents, such as tocilizumab, which targets specific inflammatory pathways and reduces long-term dependence on steroids.
Giant Cell Arteritis
With appropriate treatment, most people experience symptom relief and stabilisation. However, some patients may have relapses, requiring long-term management.
Giant cell arteritis is a medical emergency when vision is threatened, and anyone over 50 experiencing new headaches, jaw pain, or visual symptoms should seek immediate evaluation.