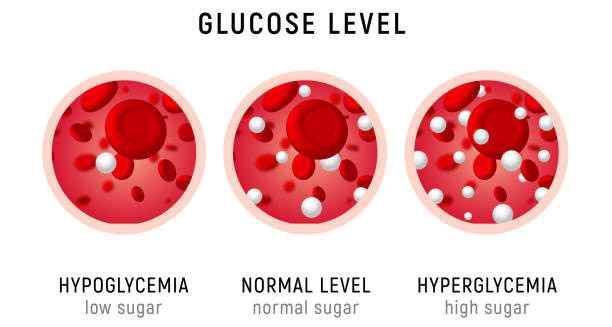
Hypoglycaemia is a medical condition marked by a low level of glucose (sugar) in the blood. Glucose is the body’s main energy source, especially for the brain. Keeping blood sugar steady is key for both body and brain function. When glucose drops too low, the body goes into an emergency state. Symptoms can range from mild confusion and shaking to seizures, loss of consciousness, or even death in severe cases. Understanding hypoglycaemia helps not only people with diabetes but anyone with health issues, metabolic disorders, or those on certain medicines.
What Is Considered Hypoglycaemia?
Clinically, hypoglycaemia means blood sugar below 70 mg/dL (3.9 mmol/L). However, some people may feel symptoms at higher or lower levels depending on their usual blood sugar and situation.
There are three main levels:
- Mild Hypoglycaemia: Hunger, shakiness, or sweating occur, but the person can treat it by eating sugar.
- Moderate Hypoglycaemia: Symptoms get stronger, like confusion, irritability, or poor coordination.
- Severe Hypoglycaemia: The person cannot function alone and may have seizures or lose consciousness.
People with hypoglycaemia unawareness do not get the usual warning signs, so monitoring is vital for them.
How the Body Maintains Blood Sugar
Normally, hormones keep blood sugar in balance. Insulin lowers blood sugar by helping cells take in glucose. Other hormones like glucagon, adrenaline, and cortisol raise blood sugar when it drops too low.
Hypoglycaemia happens when this balance breaks due to:
- Too much insulin (injected or made by the body)
- Not eating enough or fasting too long
- Hard exercise without enough fuel
- Liver or kidney problems that affect glucose production or use
In diabetes, low blood sugar is mostly caused by insulin or medication. In others, causes can be harder to find without proper checks.
Who Is at Risk?
Many people can get hypoglycaemia, especially:
- People with diabetes, especially on insulin or sulfonylureas
- Children with metabolic disorders like congenital hyperinsulinism
- Those with liver disease, which lowers glucose production
- Older adults with many health problems or on multiple drugs
- Athletes doing long endurance sports without enough carbs
- People who had weight-loss surgery (bariatric surgery) due to changed insulin control
Even healthy people can get reactive hypoglycaemia, where blood sugar falls sharply after eating because of a strong insulin response.
Signs and Symptoms
Since the brain relies on glucose, most symptoms involve the nervous system. Early signs include:
- Shaking or trembling
- Sweating
- Fast heartbeat
- Hunger
- Dizziness
- Anxiety
If blood sugar drops more, brain function is affected causing:
- Confusion
- Blurred vision
- Trouble concentrating
- Slurred speech
- Mood swings or irritability
- Seizures or unconsciousness
Catching these signs early helps prevent serious problems. People with frequent lows may lose symptom awareness, raising their risk.
Why Hypoglycaemia Is Dangerous
The brain cannot store glucose, so it is very sensitive to low sugar. Severe hypoglycaemia can cause:
- Seizures
- Loss of consciousness
- Heart rhythm problems
- Permanent brain damage
- Death, especially during sleep or when alone
Repeated episodes may harm memory, mood, and thinking, especially in kids or older adults.
The Importance of Prompt Treatment
Even mild symptoms need quick attention. Eating 15–20 grams of fast sugar (like glucose tablets, sugary drinks, or juice) can restore levels and stop worsening.
People at risk should:
- Always carry fast-acting sugar
- Wear medical ID
- Check blood sugar often
- Adjust medicine or food when sick or active
For severe lows, family may need to use emergency glucagon or call for help.
Advances in Monitoring and Prevention
Continuous glucose monitors (CGMs) alert users and caregivers to falling blood sugar before symptoms start. This reduces serious episodes in insulin users.
Smart insulin pumps and artificial pancreas systems adjust insulin automatically using real-time data, helping people with type 1 diabetes avoid lows.
Even those without diabetes benefit from CGMs or frequent testing during fasting, illness, or heavy exercise. This helps spot patterns and avoid unnoticed lows.
Conclusion
Hypoglycaemia is more than just feeling low energy or hungry. It is a serious imbalance that can disrupt health if severe or repeated. It affects people with diabetes, other health conditions, or due to diet and lifestyle.
Raising awareness, using monitoring tools, and personalising care plans are key to lowering risks. With good education and modern technology, many can predict, prevent, and manage hypoglycaemia well—keeping their independence and quality of life.
Hypoglycaemia requires quick recognition and action to stay safe.