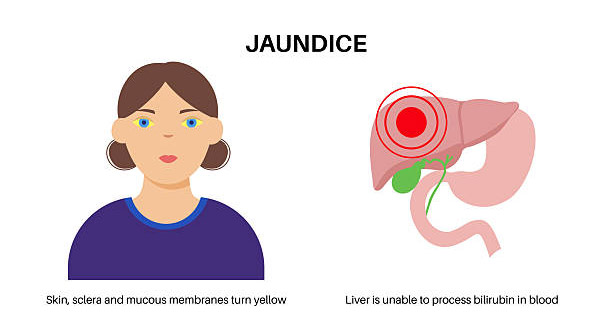
Jaundice refers to a clinical condition in which the skin, the whites of the eyes, and sometimes mucous membranes develop a yellowish discolouration. This yellowing happens because bilirubin, a yellow-orange pigment formed during red blood cell breakdown, builds up in the body. Jaundice is not a disease itself but a visible symptom of an underlying problem, usually involving the liver, gallbladder, or pancreas. Recognising jaundice is important because it often signals serious internal issues needing medical attention.
Bilirubin travels through the blood to the liver, where it is processed and then sent to the digestive tract via bile. Any disruption along this path—from red blood cell breakdown to bile excretion—can cause bilirubin to build up. Causes range from mild issues like dehydration or certain medicines to serious illnesses such as liver cirrhosis, hepatitis, or bile duct blockage. Newborns may also get jaundice because their livers are immature, which usually clears with time or light therapy.
What Happens in the Body During Jaundice?
Understanding jaundice means knowing the bilirubin cycle. Red blood cells live about 120 days. When they break down in the spleen and bone marrow, they produce unconjugated bilirubin, which does not dissolve in water. This bilirubin binds to albumin and moves to the liver. In the liver, it converts to conjugated bilirubin, which dissolves in water and flows into bile ducts. It then passes into the intestines to be excreted in stool.
Any problem in this sequence—too much red blood cell breakdown, liver damage, or bile duct blockage—raises bilirubin levels in the blood. The extra bilirubin causes the skin and eye whites to turn yellow. The urine may become dark brown because the kidneys remove excess bilirubin. Stools may look pale or clay-coloured if bile flow to the intestines is reduced or blocked.
Types of Jaundice
Doctors classify jaundice into three main types, each with different causes and treatments:
- Pre-hepatic jaundice happens when red blood cells break down too fast (haemolysis), raising unconjugated bilirubin. Sickle cell anaemia and malaria are common causes.
- Hepatic jaundice happens when the liver is sick and cannot process bilirubin well. This occurs in viral hepatitis, alcoholic liver disease, or drug-induced liver injury.
- Post-hepatic jaundice, also called obstructive jaundice, happens when bile flow is blocked after the liver. Gallstones, tumours, or bile duct narrowing cause this and raise conjugated bilirubin.
Knowing the type helps guide tests and treatments.
Who Is at Risk?
Jaundice can affect anyone but is more common in some groups:
- Newborns, especially premature babies with immature livers
- People with liver diseases like hepatitis B or C, alcoholic hepatitis, or cirrhosis
- Those with haemolytic disorders such as thalassaemia or autoimmune haemolytic anaemia
- People with a history of gallstones or pancreatitis
- Patients taking liver-toxic medicines like some antibiotics or anti-tuberculosis drugs
Older adults also face higher risk due to aging liver function and a greater chance of cancers blocking bile flow.
Common Symptoms and Clinical Presentation
Besides yellowing skin and eyes, jaundice may cause:
- Dark urine
- Pale stools
- Itching, especially in obstructive jaundice
- Fatigue and general weakness
- Abdominal pain, mainly in the upper right side
- Nausea and vomiting
- Unintended weight loss, often in cancer cases
- Fever and chills, usually with infections like hepatitis or bile duct infection
Sometimes, jaundice is the only sign in mild liver problems or haemolytic anaemia.
Diagnosis and Medical Evaluation
Doctors diagnose jaundice by examining the skin, eyes, and mucous membranes. Blood tests measure total bilirubin and separate it into unconjugated and conjugated types. Liver function tests like ALT, AST, ALP, and GGT help locate the problem. Imaging tests such as ultrasound, CT, or MRI assess the liver and bile ducts. In difficult cases, liver biopsy or endoscopic retrograde cholangiopancreatography (ERCP) may be needed to find the exact cause.
Importance of Prompt Medical Attention
Ignoring jaundice can cause serious harm. Untreated bile duct blockage can lead to infections, sepsis, or permanent liver damage. Chronic liver diseases may remain hidden until jaundice appears, signaling advanced illness. Quick diagnosis and treatment prevent long-term health problems.
Treatment Depends on the Underlying Cause
Treatment focuses on the cause, not jaundice itself. For example:
- Haemolytic anaemia needs control of red cell breakdown or infection treatment like malaria
- Hepatitis may require antiviral or immune-suppressing drugs
- Obstructive jaundice often needs surgery or stents to open blocked bile ducts
- Newborn jaundice is treated with light therapy or blood exchange
Prognosis and Outlook
The outlook depends on cause, severity, and how fast treatment starts. Neonatal jaundice usually clears quickly with little treatment. Liver failure or cancer-related jaundice can have a poor prognosis. Early detection, lifestyle changes (like reducing alcohol), and following treatment improve chances of recovery.
Preventive Strategies
To reduce jaundice risk:
- Get vaccinated against hepatitis A and B
- Drink alcohol safely or avoid it if you have liver disease
- Monitor liver health regularly if at risk
- Treat infections and gallbladder problems early
- Avoid liver-harming drugs and herbs
Public health efforts and early screening also help control jaundice in high-risk areas.
Conclusion
Overview of jaundice shows it is a symptom with many causes—from mild to life-threatening. Yellow skin and eyes may seem minor but often warn of serious problems. Quick medical evaluation, accurate diagnosis, and treatment focused on the cause are key to better outcomes and preventing complications. Understanding jaundice helps patients and doctors act quickly to manage this important sign and improve health for all ages.