Overview of Jaundice in Newborns
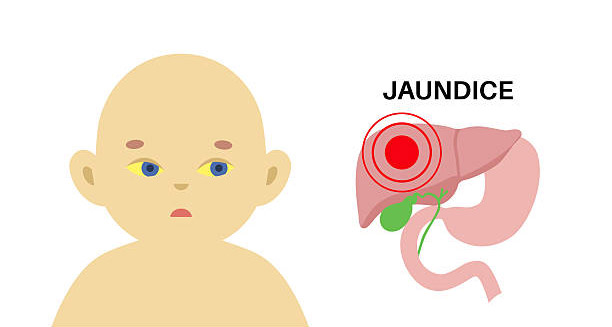
Jaundice in newborns is a widespread and often harmless condition that affects many babies in their first days of life. It causes a yellowish tint on the skin and the whites of the eyes. This happens because bilirubin levels in the blood rise. Bilirubin is a yellow pigment made when the body breaks down red blood cells.
A newborn’s liver is still immature after birth. It cannot fully process and remove bilirubin right away. In most cases, this condition—called hyperbilirubinaemia—resolves on its own without treatment. However, jaundice can sometimes signal a deeper problem or become dangerous if left untreated. If bilirubin rises too high, it can enter the brain and cause kernicterus. This rare but serious complication can lead to permanent brain damage or death. For these reasons, early recognition and treatment matter a lot.
Understanding Bilirubin and the Newborn Liver
To understand jaundice in newborns, we must look at bilirubin and how a baby’s liver works. Bilirubin forms naturally when red blood cells break down. In adults, the liver changes bilirubin into a form that dissolves in water. Then, the body removes it in stool and urine.
Newborns have immature livers that cannot process bilirubin well yet. Also, their red blood cells break down faster than adults’. On top of that, newborns lack the gut bacteria needed to help remove bilirubin through the intestines. As a result, bilirubin can build up in their blood.
This temporary imbalance usually peaks between day three and five. Then, it fades within two weeks in full-term babies. Preterm babies may take up to three weeks.
Types of Neonatal Jaundice
There are several types of jaundice in newborns. Each type needs a different approach:
- Physiological Jaundice: The most common and usually harmless type. It appears after 24 hours, peaks at day three, and fades within 7 to 14 days without treatment. It happens because the liver is immature and red blood cells break down fast.
- Breastfeeding Jaundice: Happens in the first week. It’s caused by poor feeding or dehydration, which lowers bilirubin removal. Usually improves when feeding gets better.
- Breast Milk Jaundice: Starts after the first week and lasts for several weeks. Some substances in breast milk slow bilirubin processing. It is usually harmless, so breastfeeding continues.
- Pathological Jaundice: Begins within 24 hours or lasts longer than expected. Causes include blood group incompatibility, infection, metabolic or liver problems. Needs urgent care.
- Prolonged Jaundice: Lasts more than 14 days in full-term or 21 days in preterm babies. May indicate liver disease, biliary atresia, hypothyroidism, or infection.
The timing and speed of jaundice development help doctors decide what type it is.
Risk Factors for Jaundice in Newborns
While any newborn can develop jaundice, some factors raise the chance or severity:
- Prematurity, since preterm livers are less mature
- Bruising during birth, which increases red blood cell breakdown
- Family history of jaundice
- Blood type incompatibility between mother and baby
- Poor feeding causing dehydration
- Ethnicity, as East Asian babies have a higher risk
Doctors carefully monitor babies with these risks, especially during the first week.
Clinical Signs of Jaundice
The main sign is yellow skin and eyes. This usually starts on the face and spreads downward. Natural light helps spot this color best. It may be harder to see in darker skin tones.
Other signs may include:
- Poor feeding or sleepiness
- High-pitched crying
- Weak muscle tone
- Dark yellow urine or pale stools
Most babies stay well despite jaundice, but it is vital to tell harmless cases from serious ones.
Diagnostic Tools for Jaundice
Healthcare workers check jaundice using both sight and tests:
- Transcutaneous bilirubinometer: A quick, non-invasive device that measures bilirubin through the skin.
- Serum bilirubin test: Blood sample measuring total and direct bilirubin to guide treatment.
- Coombs test: Detects blood group clashes.
- Liver and infection tests: Used when jaundice lasts long or has unknown causes.
These tests help decide if treatment is needed and prevent bilirubin from reaching dangerous levels.
Importance of Early Detection
The main risk with jaundice in newborns is that bilirubin harms the brain. Unconjugated bilirubin can cross the blood-brain barrier. This risk rises if levels climb quickly or stay high too long.
If untreated, babies can develop acute bilirubin encephalopathy and later kernicterus. Both cause permanent brain damage. Because of this, hospitals use screening programs and teach parents what to watch for before discharge.
Global and Public Health Impact
Though well-resourced hospitals handle jaundice well, it remains a major cause of newborn illness and death in poorer areas. Lack of testing tools, phototherapy, and trained staff leads to preventable harm.
Global health groups work to improve training, raise awareness, and provide basic care equipment. Early check-ups, parent education, and community outreach all help reduce complications worldwide.
Conclusion
Jaundice in newborns is common but complex. Most cases are mild and clear up naturally. Still, some reflect serious issues or risk dangerous complications. Knowing the different types, risk factors, and how to monitor and treat jaundice helps babies grow healthy.
Both clinical care and public health depend on early detection, education, and access to treatment. In the next section, we will examine the causes of jaundice in newborns in more detail.