Overview of Lipoedema
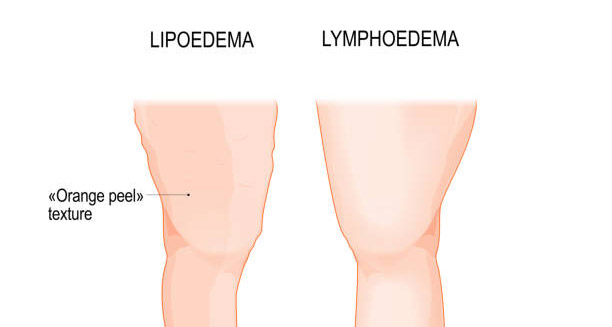
Understanding the overview of lipoedema is essential to grasp this chronic and often misunderstood condition. Lipoedema mainly affects women and causes abnormal, symmetrical fat build-up in the lower body. This includes the hips, buttocks, legs, and sometimes the arms. Unlike general obesity, lipoedema fat does not shrink with diet or exercise. This makes the condition both physically and emotionally challenging. Because lipoedema often looks like obesity or lymphoedema, it is frequently misdiagnosed. Recognising the overview of lipoedema helps raise awareness, encourages early diagnosis, and improves treatment.
Lipoedema was first described in the 1940s. Doctors noticed uneven fat in the lower body that didn’t respond to weight loss. Since then, research has grown slowly. Still, lipoedema remains underdiagnosed and misunderstood, partly because of its complex symptoms and the stigma linked to body weight. Unlike fluid retention or normal weight gain, the swelling in lipoedema starts at the hips and moves downwards—always sparing the feet. This is a key sign that helps distinguish it from other conditions.
Most people develop lipoedema during major hormonal changes like puberty, pregnancy, or menopause. This suggests hormones play a big role. While the exact cause isn’t clear, many women report family members with similar symptoms, showing a likely genetic link. An important part of the overview of lipoedema is knowing it often gets worse over time. The condition passes through stages that bring more pain, trouble moving, and possible complications such as lymphoedema, where lymph fluid builds up.
Symptoms include disproportionate fat on the lower body, painful fat deposits, easy bruising, tenderness, and a heavy feeling in the legs or arms. Many patients struggle to find clothes that fit because their upper body is slim but their lower body is much larger. Lipoedema can greatly lower quality of life, causing physical pain and emotional stress due to changes in body shape and social stigma.
Another key part of the overview of lipoedema is how it is diagnosed. Because it looks like other disorders and lacks a clear test, doctors rely on physical exams and patient history. They check fat distribution, rule out other problems like lymphoedema, and consider symptom patterns. Misdiagnosis often means years of wrong treatments and emotional pain. That’s why raising awareness among both the public and healthcare professionals is so important.
The condition also impacts mental health. Many patients suffer from anxiety, depression, and low self-esteem. They often face misunderstanding from society and even some medical staff who may dismiss their concerns. Many women endure their symptoms quietly, thinking it’s their fault or just part of aging or gaining weight. Patient groups and awareness campaigns have helped change this view, but more progress is needed.
When it comes to treatment, there is no cure yet. However, many therapies help manage symptoms and slow the disease. These include manual lymph drainage, compression garments, regular exercise, and an anti-inflammatory diet. In advanced cases, specialist liposuction can reduce fat and improve life quality. Treatment should always be personalized, addressing physical symptoms as well as emotional and social needs.
The financial cost of lipoedema can be high. Many patients pay out of pocket for special garments and therapies not covered by insurance. This lack of recognition in healthcare systems, especially in some countries, makes access to care harder. Addressing these inequalities is an important part of the bigger overview of lipoedema.
Recent research and patient advocacy have increased interest in lipoedema’s causes. Scientists are studying genes, hormones, blood vessel problems, and connective tissue issues. More funding for research and clinical trials is needed. This work will help create better diagnostic tools and treatments. Advancements could greatly improve lives and reduce stigma.
In summary, the overview of lipoedema offers a clear picture of a complex, often overlooked disease. By telling lipoedema apart from obesity and swelling, doctors can diagnose it accurately and offer better care. Patients who understand the overview of lipoedema can better advocate for themselves, seek the right treatments, and connect with others. As awareness grows, hope increases for better outcomes and more research into this important condition.