Overview of Lupus
Lupus is a chronic, systemic autoimmune disease in which the immune system mistakenly attacks healthy tissues and organs. This abnormal immune response causes widespread inflammation, pain, and potential damage in areas such as the skin, joints, kidneys, brain, heart, lungs, and blood cells.
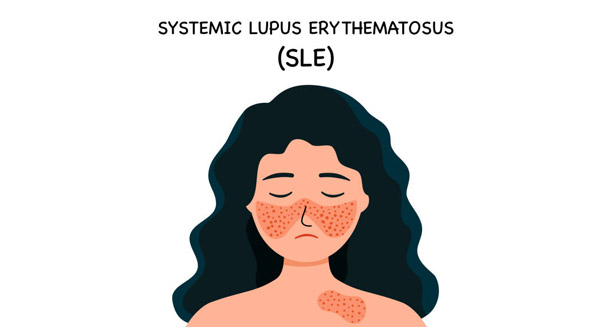
The most common and widely studied form is Systemic Lupus Erythematosus (SLE), but there are other types:
- Cutaneous, affecting only the skin
- Drug-induced, triggered by certain medications
- Neonatal, a rare condition seen in newborns of mothers with specific autoantibodies
This overview provides essential context on the nature, scope, and complexity of lupus, a condition that affects millions worldwide.
What Is Lupus? Understanding the Autoimmune Nature
In a healthy immune system, the body defends against harmful invaders like viruses and bacteria. In lupus, this defence system becomes misguided — it fails to distinguish between foreign invaders and the body’s own cells. This leads to the production of autoantibodies, which mistakenly attack the body’s tissues.
This core mechanism explains the multi-organ impact and unpredictable nature of lupus — and why it can be so difficult to diagnose and manage.
The Unpredictability of Lupus
One of lupus’s most defining characteristics is its relapsing-remitting course. This means:
- Flares: Periods when symptoms worsen or new symptoms appear
- Remission: Times when symptoms lessen or disappear
These flares can vary greatly in intensity, duration, and organ involvement, making this condition notoriously difficult to predict. Because of this variability, lupus is often referred to as “the great imitator”, as its symptoms mimic many other diseases.
Who Gets Lupus?
Lupus can affect anyone, but it is most common in:
- Women of childbearing age (15–45 years)
- People with a family history of lupus or other autoimmune disorders
- Certain ethnic groups, including individuals of African, Asian, Hispanic, or Native American descent
This pattern suggests that this condition results from a combination of genetic, hormonal, and environmental factors.
Common Symptoms of Lupus
Symptoms can be mild to severe and may change over time. The most frequently reported symptoms include:
- Chronic fatigue
- Joint pain and swelling, especially in the hands and knees
- Skin rashes, particularly the butterfly-shaped malar rash across the cheeks and nose
- Fever
- Hair loss
- Photosensitivity
- Mouth or nose ulcers
More serious manifestations include:
- Kidney inflammation (lupus nephritis)
- Neurological symptoms, such as seizures or memory problems
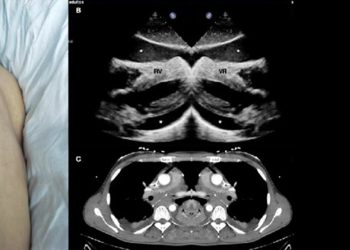
- Heart and lung inflammation (pericarditis, pleuritis)
Because symptoms vary so widely, lupus often requires multidisciplinary care involving rheumatologists, nephrologists, dermatologists, and other specialists.
How Is Lupus Diagnosed?
There is no single test for lupus. Diagnosis is based on a combination of:
- Clinical evaluation of signs and symptoms
- Laboratory tests, including:
- Antinuclear antibody (ANA) test
- Anti-dsDNA and anti-Smith antibodies
- Blood counts, ESR, CRP
- Urinalysis to detect kidney involvement
- Imaging studies and sometimes biopsies to assess organ damage
Doctors may use criteria from organisations like the American College of Rheumatology (ACR) or EULAR/ACR 2019 classification to guide diagnosis.
Lupus Treatment and Management
There is no cure for lupus, but the disease can be managed through a combination of medications and lifestyle adjustments. Treatment aims to:
- Control symptoms
- Prevent flares
- Protect organs from damage
- Improve quality of life
Treatment options may include:
- NSAIDs for pain and inflammation
- Antimalarials (e.g., hydroxychloroquine) to manage symptoms and prevent flares
- Corticosteroids to reduce inflammation quickly
- Immunosuppressants for more severe cases
- Biologics, such as belimumab, to target specific immune pathways
Ongoing research is bringing new targeted therapies with fewer side effects to the forefront of lupus care.
Self-Management and Lifestyle
Effective lupus care goes beyond medication. Patients are encouraged to:
- Avoid direct sunlight and wear high-SPF sunscreen
- Get adequate rest to manage fatigue
- Eat a balanced, anti-inflammatory diet
- Engage in light exercise to improve joint mobility and mood
- Manage stress, a known trigger for flares
- Avoid smoking and limit alcohol
Regular medical check-ups and early intervention are key to preventing complications.
Emotional and Social Impact
Living with lupus can be emotionally challenging. Many patients experience:
- Depression and anxiety
- Social isolation
- Financial stress due to medical expenses and reduced ability to work
Support groups, counselling, and education can greatly improve emotional well-being and empower patients to manage their condition effectively.
Research and Future Outlook
The outlook for people with lupus has improved significantly over the past few decades. Current research focuses on:
- Understanding immune pathways
- Developing better diagnostic tools
- Creating safer and more effective treatments
- Discovering potential biomarkers for early detection
Increased awareness, early diagnosis, and a personalised approach to care are helping more people with lupus lead full, active lives.
Summary: What Is Lupus?
Lupus is a chronic autoimmune condition with diverse symptoms and an unpredictable course. Early recognition, multidisciplinary care, and tailored treatment are crucial for managing lupus effectively. With ongoing medical advancements and greater public awareness, the future is increasingly hopeful for people living with lupus.