Treatment of Gynaecomastia
The treatment of gynaecomastia depends on the cause, duration, severity, and impact on a person’s physical and emotional wellbeing. In many cases, the treatment of gynaecomastia is not required, as the condition may resolve on its own. However, persistent or distressing cases often warrant medical or surgical intervention to address symptoms and restore confidence.
Gynaecomastia is the benign enlargement of male breast tissue due to hormonal imbalance, particularly an increased ratio of oestrogen to testosterone. It can affect males of all ages — from newborns to older men — and may be unilateral or bilateral. While not life-threatening, the psychological impact can be significant.
1. Observation and Reassurance
In many adolescents and some adults, gynaecomastia is:
Physiological (a normal part of development)
Transient, resolving within 6 to 12 months
Associated with no underlying disease
In such cases, doctors may recommend:
Monitoring without intervention
Regular follow-up to ensure the condition is improving or stabilising
Reassurance that it is common and often temporary
This approach is especially appropriate for teenage boys during puberty, where as many as 60% may experience some degree of breast enlargement.
2. Addressing Underlying Causes
Secondary gynaecomastia caused by medical conditions or medications requires treatment of the root issue. This includes:
Discontinuing or replacing drugs known to cause gynaecomastia (e.g. spironolactone, anti-androgens, anabolic steroids)
Managing hormonal disorders, such as hypogonadism or hyperthyroidism
Treating liver or kidney disease that may alter hormone metabolism
Stopping the use of recreational drugs such as cannabis or alcohol
Doctors will often perform blood tests to assess hormone levels and organ function when secondary causes are suspected.
3. Medical Therapy
Medical treatment is most effective in the early, active phase of gynaecomastia, when breast tissue is still proliferating (within 6–12 months of onset).
a. Selective Oestrogen Receptor Modulators (SERMs)
Tamoxifen is commonly used to reduce breast tissue size and tenderness
Works by blocking oestrogen receptors in breast tissue
Often used off-label with encouraging results
Generally well tolerated but may cause fatigue or hot flushes
b. Aromatase Inhibitors
Anastrozole or letrozole reduce oestrogen production
Less effective than tamoxifen for established gynaecomastia
Reserved for specific cases with hormonal abnormalities
c. Androgens or Testosterone Therapy
May help in cases of testosterone deficiency
Only used if there is a clear diagnosis of hypogonadism
Should be carefully monitored to avoid adverse effects
Medical therapy is rarely effective in long-standing fibrotic gynaecomastia, where the tissue becomes firm and unresponsive to hormonal treatment.
4. Surgical Treatment
Surgery is considered the definitive treatment of gynaecomastia, particularly in cases of:
Persistent enlargement despite medical therapy
Psychological distress or body image concerns
Pain or tenderness
Excess skin or large-volume tissue, especially in older adults or those with massive weight loss
There are two main surgical options:
a. Liposuction
Ideal for cases with fat-dominant breast tissue
Involves suctioning excess fat through a small incision
Less invasive, quicker recovery
Limited ability to remove glandular tissue
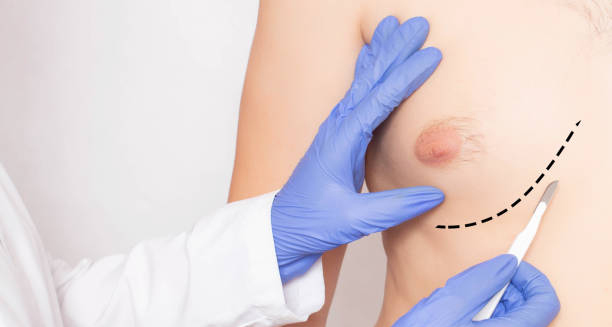
b. Excisional Surgery (Mastectomy)
Involves direct removal of glandular tissue via a small incision around the areola
Sometimes combined with liposuction for optimal contouring
More effective for firm, fibrous, or long-standing tissue
Recovery from surgery typically involves:
Wearing compression garments
Managing swelling and bruising
Returning to work within 1 to 2 weeks
Scarring is minimal and usually fades over time. Most patients report high satisfaction post-surgery.
5. Psychological and Supportive Care
The emotional effects of gynaecomastia should not be underestimated. Many affected individuals experience:
Low self-esteem
Social withdrawal
Avoidance of sports or swimming
Anxiety or depression
Supportive strategies include:
Counselling or cognitive behavioural therapy (CBT)
Support groups for men with body image issues
Education about the condition to reduce stigma
Treating the psychological aspects can be just as important as addressing the physical symptoms.
6. Lifestyle Measures
Certain lifestyle adjustments may support overall management:
Weight loss and exercise can reduce chest fat and improve appearance, though they do not affect glandular tissue
Avoiding alcohol and drugs known to impact hormone levels
Healthy eating to support hormone balance and body confidence
However, it’s important not to falsely promise resolution through diet and exercise alone when true glandular gynaecomastia is present.
Conclusion | Treatment of Gynaecomastia
The treatment of gynaecomastia can range from simple observation to medical and surgical interventions, depending on the cause and severity. While many cases resolve naturally, persistent or emotionally distressing gynaecomastia may require hormone therapy or surgery. A holistic approach to the treatment of gynaecomastia, addressing both physical and psychological aspects, offers the best outcomes for patients seeking relief and restoration of confidence.