Causes and Risk Factors of Actinomycosis
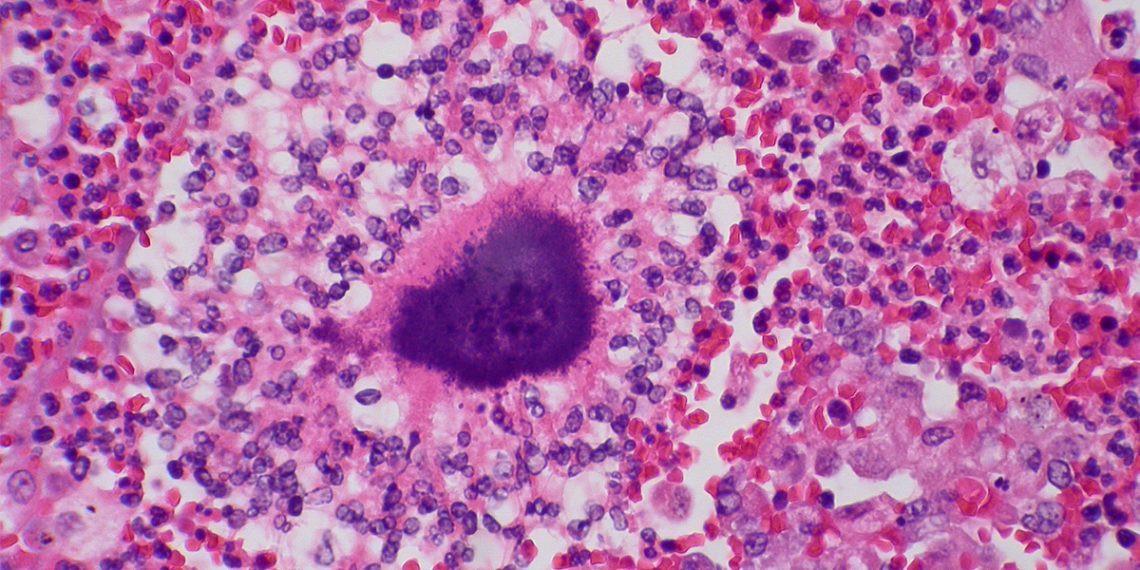
The causes and risk factors of actinomycosis revolve around how Actinomyces bacteria, which usually live harmlessly in the mouth, throat, and gut, gain access to deeper body tissues. These bacteria become dangerous only when they invade areas where they don’t belong. This usually happens after trauma, infection, or surgical procedures that break the protective barriers of the body. Once inside, the bacteria trigger slow-growing infections that often mimic other diseases.
How the Infection Begins
Dental procedures are one of the most common entry points. Tooth extractions, gum disease, or untreated cavities allow the bacteria to move into facial tissues. As a result, cervicofacial actinomycosis — often called “lumpy jaw” — may develop, especially in those with poor oral hygiene or recent dental work.
In the abdomen, trauma or gastrointestinal surgery can lead to infections. Conditions like diverticulitis sometimes cause bowel perforation. This lets bacteria escape the gut and spread into nearby tissues, forming abscesses that become difficult to treat.
Thoracic actinomycosis usually follows pulmonary aspiration. This is more common in people who smoke, drink heavily, or maintain poor oral hygiene. Infections may settle in the lungs and mimic diseases like tuberculosis or lung cancer.
Pelvic actinomycosis affects women who use intrauterine devices (IUDs) for longer than five years without monitoring. In these cases, bacteria colonise the device and spread to the surrounding organs, creating masses that resemble gynaecological cancers.
Major Risk Factors
- Poor oral hygiene and untreated dental infections
- Abdominal trauma or previous gastrointestinal surgery
- Prolonged IUD use without follow-up
- Immunocompromised states such as HIV or diabetes
- Malnutrition or poverty, particularly in rural areas of South Africa
Local Challenges in South Africa
In South Africa, the causes and risk factors of actinomycosis often go unnoticed, particularly in primary healthcare settings. Unfortunately, many clinics still lack immediate access to reliable diagnostic tools. As a result, healthcare workers often rely on clinical signs alone, which can be misleading. Since symptoms of actinomycosis frequently resemble more common conditions like tuberculosis or cancer, doctors may easily misdiagnose the infection.
Consequently, patients often receive inappropriate or delayed treatment, which allows the disease to progress further. In some cases, they undergo unnecessary surgical procedures or months of incorrect medication. Over time, this not only worsens patient outcomes but also places added pressure on an already strained healthcare system.
Therefore, raising awareness among healthcare providers is essential. Targeted training and clinical education can help frontline staff recognise early signs of actinomycosis and consider it as a differential diagnosis. With faster recognition, patients are more likely to receive the right tests and treatments early on.
Ultimately, early diagnosis can prevent severe complications, reduce hospital stays, and avoid unnecessary surgery. Most importantly, it can improve long-term recovery outcomes for patients — especially in rural and underserved communities across the country.
Causes and Risk Factors of Actinomycosis
🔹 Next → [Symptoms and Types of Actinomycosis]