Diagnosis of Cardiovascular Disease
Diagnosis of cardiovascular disease involves a combination of physical examination, risk assessment, and diagnostic testing. A correct diagnosis allows for timely treatment and helps prevent life-threatening complications.
Doctors start by evaluating medical and family history, lifestyle habits, and symptoms. They measure blood pressure, listen to the heart, and check for signs of poor circulation or fluid retention.
Common tests include:
1. Blood Tests
- Cholesterol levels (LDL, HDL, triglycerides)
- Blood sugar and HbA1c for diabetes
- Cardiac enzymes like troponin (especially during suspected heart attack)
- BNP levels for heart failure
2. Electrocardiogram (ECG)
Measures the heart’s electrical activity and helps detect arrhythmias, previous heart attacks, or abnormal rhythms.
3. Echocardiogram
An ultrasound of the heart that shows structure, pumping function, and valve function. It is key for diagnosing heart failure and valve disease.
4. Stress Tests
Evaluate heart performance under exertion. These may involve walking on a treadmill or taking a medication that stresses the heart while monitoring ECG and imaging.
5. Coronary Angiography
A dye is injected into the coronary arteries and visualised with X-rays to detect blockages. It is used for assessing coronary artery disease.
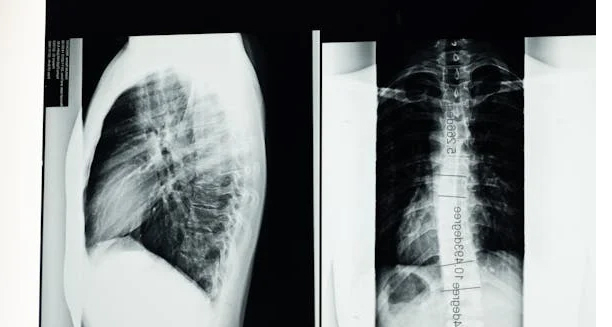
6. CT or MRI Scans
Advanced imaging tools used to assess plaque build-up, congenital defects, or damage after a heart event.
7. Holter Monitor or Event Recorder
Diagnosis of Cardiovascular Disease
Worn for 24–72 hours or longer to detect intermittent heart rhythm problems.
A full diagnosis of cardiovascular disease provides a foundation for personalising treatment, determining risk, and establishing long-term management goals.
[Next: Treatment of Cardiovascular Disease →]