Complications of Haemochromatosis
The complications of haemochromatosis occur when excess iron builds up in organs and tissues, leading to damage over time. If left untreated, the complications of haemochromatosis can be severe and include liver cirrhosis, diabetes, heart disease, arthritis, and hormonal imbalances. Fortunately, early diagnosis and treatment can prevent or limit most of these outcomes.
Haemochromatosis causes the body to absorb more iron than it needs. Over years, this iron accumulates silently, as the body has no natural mechanism to excrete excess iron efficiently. Once stores exceed safe levels, iron begins to deposit in vital organs, disrupting their normal function and potentially leading to life-threatening illness.
1. Liver Complications
The liver is one of the first organs affected by iron overload.
Common liver-related complications:
Hepatomegaly (enlarged liver)
Fibrosis (scarring)
Cirrhosis – a significant risk factor for liver failure and liver cancer
Hepatocellular carcinoma (HCC) – a rare but serious consequence of long-term iron overload
Patients with cirrhosis require:
Regular imaging (ultrasound)
Blood tests (alpha-fetoprotein) to screen for liver cancer
Avoidance of alcohol and hepatitis co-infection
Liver damage may be partially reversible if treatment begins before cirrhosis develops.
2. Diabetes and Pancreatic Dysfunction
Iron deposits in the pancreas disrupt insulin production, leading to type 2 diabetes mellitus.
Symptoms include:
Increased thirst and urination
Fatigue and blurred vision
Weight changes
Known as “bronze diabetes” when combined with skin pigmentation changes, this complication may require insulin therapy or oral hypoglycaemic agents. Even after iron levels are controlled, pancreatic damage may persist.
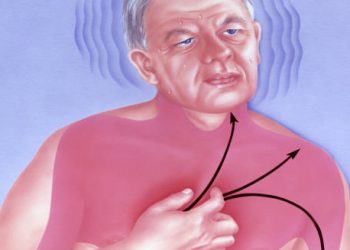
3. Heart Complications
Excess iron can infiltrate the heart muscle, leading to:
Cardiomyopathy – weakening of the heart muscle
Arrhythmias – irregular heart rhythms
Heart failure – reduced pumping efficiency
These complications may cause:
Breathlessness
Swelling in the legs
Fatigue and reduced exercise tolerance
Treatment includes iron removal, cardiac medications, and in some cases, implantable devices like pacemakers.
4. Joint and Musculoskeletal Problems
Iron can accumulate in the joints, particularly the hands, hips, and knees.
Common issues:
Arthropathy (joint disease)
Osteoarthritis-like symptoms
Stiffness and chronic pain
Reduced grip strength
Unfortunately, joint symptoms often do not improve even after iron reduction, making pain management and physiotherapy important.
5. Skin Discolouration
Iron deposits in the skin can cause:
Grey-brown or bronze pigmentation
Often noticeable on the face, neck, and forearms
This gives rise to the term “bronze diabetes” when combined with glucose intolerance. Skin tone often improves with ongoing treatment.
6. Hormonal and Sexual Dysfunction
Iron affects hormone-producing glands, particularly the pituitary gland, resulting in:
Hypogonadism – reduced sex hormone production
Erectile dysfunction or reduced libido
Amenorrhoea or infertility in women
Thyroid and adrenal gland dysfunction (less common)
Hormone replacement therapy may be needed in these cases.
7. Fatigue and Cognitive Issues
Fatigue is one of the most commonly reported symptoms, even in early stages:
May persist even after iron levels normalise
Possibly due to long-term inflammation or organ damage
Affects quality of life, work, and mental health
Some patients report:
Brain fog
Concentration difficulties
Mood changes
These issues may improve with treatment but often require holistic care.
8. Increased Risk of Certain Infections
Iron is essential for bacterial growth. Excess iron may predispose individuals to infections, including:
Listeria monocytogenes
Yersinia enterocolitica
Vibrio vulnificus
These pathogens thrive in iron-rich environments, particularly in those undergoing iron chelation therapy. Awareness and appropriate hygiene precautions are important.
9. Long-Term Disability
If complications are not managed in time, they may lead to:
Permanent organ dysfunction
Reduced mobility
Dependence on medication or assistive devices
Shortened life expectancy
Late-stage diagnosis often involves multiple overlapping complications.
Preventing Complications
The best way to avoid these outcomes is through:
Early detection
Regular phlebotomy
Routine monitoring of iron and organ function
Family screening to identify at-risk relatives
Even those with early organ damage may stabilise or improve with consistent management.
Conclusion | Complications of Haemochromatosis
The complications of haemochromatosis can affect many parts of the body. If the condition is not treated early, extra iron can build up and damage important organs like the liver, heart, pancreas, and joints. Over time, this may lead to serious problems such as liver disease, heart issues, diabetes, arthritis, and hormone imbalances.
However, with early diagnosis and regular treatment—such as blood removal (phlebotomy) to lower iron levels—most of these complications can be prevented or even reversed. That’s why routine check-ups and blood tests are so important, especially for people with a family history of the condition.
By learning about the possible complications, patients and healthcare providers can work together to catch problems early, plan better care, and support long-term health.