Hyperparathyroidism happens when the parathyroid glands make too much parathyroid hormone (PTH). This hormone controls calcium and phosphorus in the body. When PTH levels stay high, blood calcium also rises. This leads to hypercalcaemia, a key sign of the condition.
The reasons for this hormone surge vary by type: primary, secondary, or tertiary hyperparathyroidism. Knowing the cause helps doctors choose the right treatment. In this section, we explain what causes hyperparathyroidism and how each type develops.
Primary Hyperparathyroidism: Gland Problems
Primary hyperparathyroidism starts when the parathyroid glands themselves go wrong. They release PTH even when calcium levels are normal or high. The main reasons include:
1. Parathyroid Adenoma
This is a non-cancerous growth on one gland. It causes that gland to stay overactive and make too much PTH. This problem is the main cause of primary hyperparathyroidism in most cases. It can lead to kidney stones, weak bones, and mental changes.
2. Parathyroid Hyperplasia
Here, all four glands enlarge and make extra hormone. This may happen alone or with genetic issues like Multiple Endocrine Neoplasia (MEN). Unlike an adenoma, this form is more widespread.
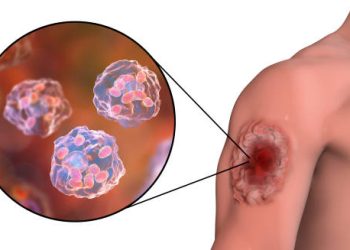
3. Parathyroid Cancer
This is very rare. When it occurs, calcium levels become very high, and symptoms can turn severe. Surgery is often needed right away.
Secondary Hyperparathyroidism: Body’s Response to Imbalance
Secondary hyperparathyroidism develops when low calcium or vitamin D levels push the glands to work harder. The glands themselves are normal, but they react to outside triggers. Main causes include:
1. Chronic Kidney Disease (CKD)
Damaged kidneys fail to activate vitamin D and cannot clear phosphate. This lowers calcium and raises phosphate, which makes PTH rise. Over time, the glands become bigger and more active.
2. Vitamin D Lack
Without enough vitamin D, the gut cannot absorb calcium well. This drop in calcium forces the glands to produce more PTH. Low vitamin D can come from little sun, gut issues, or poor diet.
3. Low Calcium Intake
Not eating enough calcium or poor gut absorption can also lower blood calcium. The glands respond by pumping out more PTH.
Tertiary Hyperparathyroidism: Loss of Control
Tertiary hyperparathyroidism often follows years of secondary disease. Even after fixing the original cause, such as after a kidney transplant, the glands stay overactive. They keep making PTH on their own. This leads to very high calcium levels and usually needs surgery.
Genetic Causes
Some cases run in families. Two main examples are:
1. Multiple Endocrine Neoplasia (MEN)
MEN1 mutations raise the risk of growths in endocrine glands, including the parathyroids. Symptoms often appear young, sometimes in the 20s.
2. Familial Hypocalciuric Hypercalcaemia (FHH)
This rare inherited condition makes the glands misread calcium levels. PTH stays high even when calcium is high. FHH is harmless and does not need surgery, unlike other forms.
Lifestyle and Other Risk Factors
Certain habits and conditions can make things worse:
• Sitting too much, which weakens bones
• Eating lots of phosphate from processed foods
• Heavy drinking or smoking, which harm vitamin D use
• Drugs like lithium or water pills, which change calcium control
• Older age, which alters gland function
These do not usually cause hyperparathyroidism alone but can add to the risk.
When Causes Mix
Sometimes the lines blur. A person with kidney disease may later develop gland changes that act like primary disease. Another person may have both low vitamin D and a gland adenoma. Careful tests and scans help find the main problem so doctors can plan treatment.
Summary
The causes of hyperparathyroidism differ by type. Primary comes from gland changes like adenomas. Secondary happens when low calcium or vitamin D makes glands overwork. Tertiary appears after long-term stress on the glands, turning them autonomous.
Finding the exact cause is key for treatment. This prevents needless surgery and helps correct the real problem early.