Causes of Gastroparesis
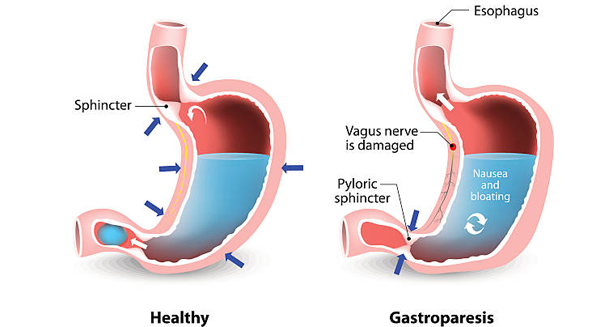
Gastroparesis occurs when the stomach’s normal muscle or nerve function becomes disrupted, preventing food from moving efficiently through the digestive tract. This dysfunction stems from various underlying conditions, each affecting the digestive system in different ways.
Diabetes
Among all known causes, diabetes stands out as the most common contributor to gastroparesis. Over time, persistently high blood sugar levels can damage the vagus nerve, which plays a crucial role in triggering the stomach’s muscle contractions. As the nerve weakens, stomach motility slows down significantly.
In addition to nerve damage, high blood sugar levels interfere with the body’s digestive hormones, further hindering the emptying process. People with poorly controlled type 1 or type 2 diabetes are especially at risk.
Idiopathic (Unknown Cause)
In many instances, no identifiable cause is found, which leads to a diagnosis of idiopathic gastroparesis. Even though the exact trigger remains unclear, experts suspect that subtle nerve damage, autoimmune responses, or even lingering effects from viral infections could be responsible. Unfortunately, without a clear origin, treatment often focuses solely on managing symptoms.
Post-Surgical Nerve Injury
Certain surgical procedures can inadvertently damage the nerves responsible for stomach function. For example, operations involving the stomach, oesophagus, or adjacent organs may lead to gastroparesis if nerves such as the vagus nerve are affected.
This scenario is especially common following surgeries like bariatric surgery, vagotomy, or fundoplication, where the risk of nerve disruption is significantly higher. In such cases, gastroparesis symptoms may appear after the body heals from surgery.
Neurological and Autoimmune Disorders
Several neurological and autoimmune conditions interfere with the stomach’s ability to function normally. These include:
- Parkinson’s disease
- Multiple sclerosis (MS)
- Amyloidosis
- Systemic sclerosis
Each of these disorders impairs either the nerve signals or muscle responses required for proper digestion, often leading to chronic delays in gastric emptying.
Viral Infections
Sometimes, gastroparesis develops after a viral illness. Infections such as Epstein-Barr virus, cytomegalovirus, or rotavirus have been linked to either temporary or long-term digestive disruptions. Some individuals begin experiencing symptoms only after recovering from a stomach bug or respiratory infection, suggesting a post-viral onset of the condition.
Medications
Certain medications are known to slow down gastric emptying, particularly:
- Opioids
- Anticholinergics
- Calcium channel blockers
In drug-induced cases, stopping or replacing the medication often leads to noticeable improvement. Therefore, identifying and addressing medication-related triggers is a key step in managing gastroparesis effectively.
Causes of Gastroparesis
Gaining a deeper understanding of what causes gastroparesis is essential for developing the most effective treatment plan. By identifying the underlying trigger—whether it’s diabetes, nerve damage, medication, or an unknown factor—healthcare providers can tailor interventions that not only relieve symptoms but also address the root cause.