Causes of Henoch-Schönlein Purpura
The causes of Henoch-Schönlein purpura (HSP) are not completely understood. Furthermore, the condition is believed to result from an abnormal immune response that leads to inflammation in the small blood vessels. Although HSP is not directly contagious or hereditary in most cases. It frequently occurs following an infection—suggesting that environmental and immunological factors play key roles. Unravelling the causes of Henoch-Schönlein purpura is essential for understanding how the disease develops and why certain individuals, particularly children, are more vulnerable.
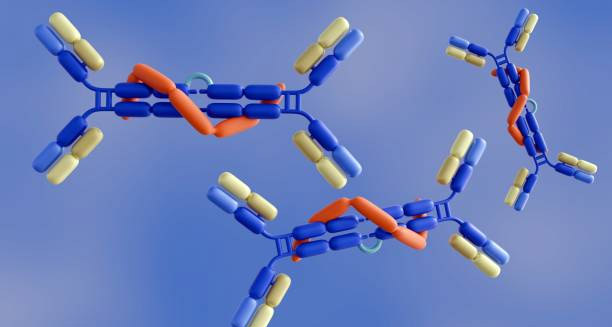
The most commonly associated trigger is an upper respiratory tract infection. Typically a viral illness such as a cold or influenza. In some cases, streptococcal infections, such as strep throat, cause the problem. The condition often arises one to three weeks after the resolution of the initial infection. Supporting the theory that the body’s immune response—rather than the pathogen itself. Is responsible for initiating the cascade of inflammation. During this process, the immune system produces elevated levels of immunoglobulin A (IgA). Which then deposit in the walls of small blood vessels, especially in the skin, joints, intestines, and kidneys.
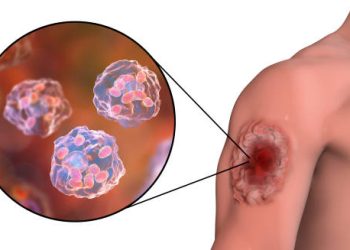
These IgA deposits cause the blood vessels to become inflamed—a process known as vasculitis. Leading to leakage of blood and proteins into surrounding tissues. This immune complex-mediated response is what produces the hallmark rash. As well as the joint, gastrointestinal, and renal symptoms commonly seen in HSP. While it is not entirely clear why the immune system reacts in this way. It may be that the body mistakenly identifies its own blood vessel components as threats following exposure to a virus or bacterium.
Causes of Henoch-Schönlein Purpura
Beyond infections, several other environmental and immunological triggers have been associated with Henoch-Schönlein purpura, although none are confirmed as direct causes. These include:
Bacterial infections, such as Helicobacter pylori or Group A streptococcus
Vaccinations, particularly those administered close in time to illness onset, including MMR (measles, mumps, rubella), influenza, and hepatitis B—though these are rare and do not outweigh the benefits of vaccination
Insect bites or stings, which may provoke an immune response in some individuals
Exposure to cold weather, which is frequently observed before flare-ups, especially in children
Certain medications, including antibiotics (like penicillin), non-steroidal anti-inflammatory drugs (NSAIDs), and ACE inhibitors, which may act as immune triggers
Although doctors see these factors in some cases, most people who have them do not get HSP. This shows that a person’s genes and how their immune system reacts probably help decide if they get the disease. Some researchers think an unknown gene may cause certain people to make too much or the wrong kind of IgA when the environment triggers them.
Interestingly, Henoch-Schönlein purpura is far more common in children, particularly those aged 2 to 11 years. This may be because their immune systems are still developing and are more reactive to pathogens. The immune systems of young children may be more prone to producing excessive IgA or to generating intense inflammatory responses to common viruses and bacteria. That said, while rare, HSP can occur in adolescents and adults, where it is often more severe—especially in terms of kidney involvement.
Causes of Henoch-Schönlein Purpura
In adults, the causes may sometimes differ slightly or be less obvious. HSP in adults is more often associated with medications, chronic infections, or autoimmune conditions. In these cases, the disease may present more aggressively and may carry a greater risk of complications, such as long-term kidney damage. The role of immune dysregulation becomes more pronounced in older individuals, especially those with coexisting autoimmune conditions like systemic lupus erythematosus or inflammatory bowel disease.
In addition to environmental and immunological factors, there is growing interest in the role of the gut microbiome in regulating immune responses, especially in children. Disruptions in gut bacteria, whether from diet, antibiotics, or infections, could contribute to immune system misfires, including overproduction of IgA. Although still speculative, this area of research may help explain why some children develop HSP following common illnesses while others do not.
The seasonality of Henoch-Schönlein purpura also provides clues about its causes. The condition is diagnosed more often in autumn and winter because respiratory viruses spread more during these seasons.. This seasonal trend supports the theory that HSP is commonly a post-infectious immune phenomenon rather than a disease with a singular direct cause.
In rare instances, familial clustering of HSP has been observed, suggesting that there may be a genetic component in some cases. However, this is the exception rather than the rule. The vast majority of individuals with HSP have no family history of the disease, and the risk of recurrence in siblings or offspring is extremely low.
Finally, it’s important to know that Henoch-Schönlein purpura does not come from poor hygiene, diet, or lifestyle, and it is not contagious. Parents, caregivers, and patients can feel reassured because the condition is not caused by anything they did wrong, and it cannot spread through casual contact.
Causes of Henoch-Schönlein Purpura
In summary, the causes of Henoch-Schönlein purpura are multifactorial and not yet fully understood. Many people believe the condition happens because the immune system overreacts, usually after a respiratory infection. Genetics, the environment, and how sensitive the immune system is also play a part. While the exact cause may remain elusive in individual cases. Understanding the various factors that can initiate the disease is crucial for early recognition and effective management.