Diagnosis of Anaphylaxis
Anaphylaxis is a clinical diagnosis — meaning it is based primarily on recognising signs and symptoms. Since the reaction progresses quickly, healthcare providers must act on presentation and history, not wait for test results.
Clinical Signs
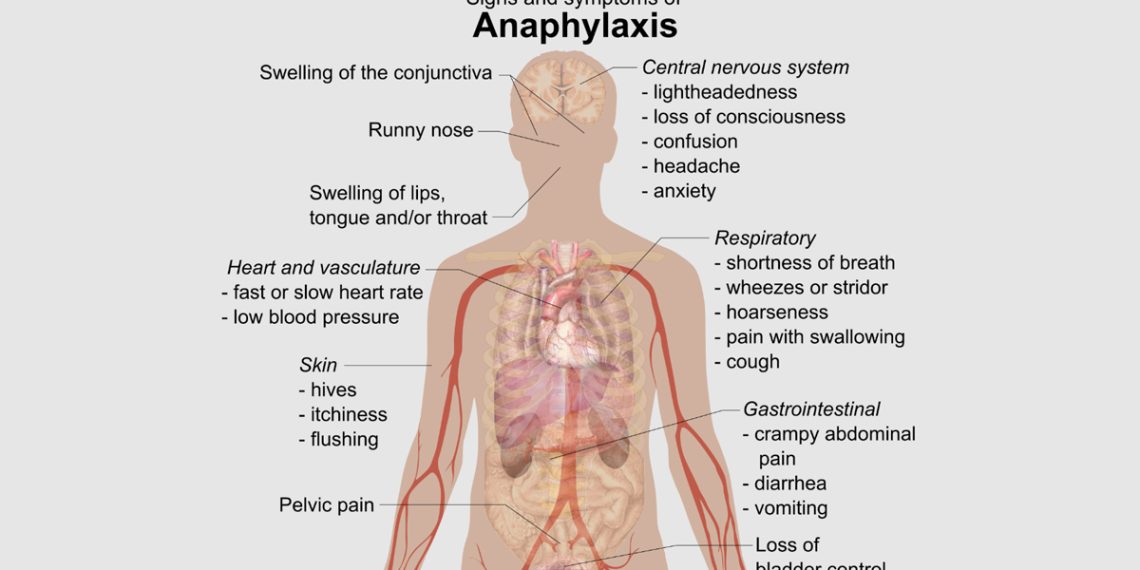
A diagnosis is strongly suspected if a person shows:
- Sudden symptoms involving the skin or mucosa (e.g. hives, swelling, itching) AND one or more of the following:
- Respiratory difficulty (wheezing, stridor, throat tightness)
- Low blood pressure or fainting
- Gastrointestinal symptoms (nausea, cramps, diarrhoea)
History and Timing
Doctors will ask about:
- Recent exposure to known allergens (food, insect sting, drug)
- Past history of allergies or anaphylaxis
- Time of onset (usually within minutes of exposure)
Physical Examination
May reveal:
- Pale or bluish skin (cyanosis)
- Swollen lips or tongue
- Rapid or weak pulse
- Wheezing or stridor
- Low blood pressure
Tests (usually done after the emergency)
- Tryptase blood test – helps confirm anaphylaxis after the event
- Allergy testing (skin prick or IgE blood tests) – helps identify the trigger
- Challenge tests – done in specialist allergy centres under supervision
In South Africa, testing may be referred to an allergist or immunologist, especially for people with recurrent or idiopathic anaphylaxis. Early diagnosis helps prevent future episodes through avoidance and emergency planning.
Next, let’s examine how to treat anaphylaxis effectively.
👉 [Next: Treatment for Anaphylaxis]
Royal Paediatrics and Allergy Claremont