Diagnosis of Henoch-Schönlein Purpura
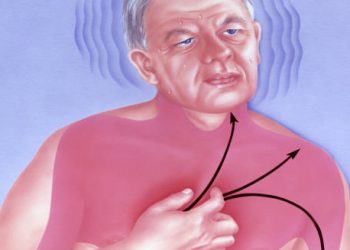
The diagnosis of Henoch-Schönlein purpura (HSP) is primarily clinical. Meaning it is based on the patient’s history and the appearance of characteristic symptoms rather than on a single definitive test. The condition typically presents with a distinctive purpuric rash. Raised purple or red spots that do not blanch when pressed—most often on the lower limbs and buttocks. When this rash occurs alongside joint pain, abdominal symptoms, or kidney involvement, the clinical picture becomes even more suggestive. Making an accurate diagnosis of Henoch-Schönlein purpura is important not only for immediate management but also for guiding follow-up care. Especially to monitor for potential kidney complications.
Clinicians begin by taking a thorough medical history, asking when the rash appeared. Whether the patient has experienced a recent respiratory illness, and if there are other symptoms such as stomach pain, vomiting, joint aches, or dark or frothy urine. A physical examination focuses on identifying the hallmark rash and checking for swelling or tenderness in the joints. The pattern and feel of the purpura are very specific in HSP. Usually, the spots can be felt as raised bumps and appear evenly on both legs and the buttocks.
In many cases, especially with children, the signs clearly show HSP, so doctors do not need to run extra tests to confirm it. But since other conditions can look like HSP—especially in adults—doctors often run additional tests to rule out other causes and check for internal problems. These tests include:
Diagnosis of Henoch-Schönlein Purpura
Blood Tests
While no blood test can definitively diagnose HSP, several can support the diagnosis or help rule out other causes of purpura and systemic illness:
Full blood count (FBC): May show a mild elevation in white blood cells or platelets, which are common in inflammatory conditions.
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are tests that show inflammation in the body. These markers often rise a little in people with HSP.
Renal function tests: Including blood urea nitrogen (BUN) and creatinine, to assess for kidney involvement.
Coagulation studies: To rule out bleeding disorders if purpura is present without other typical features of HSP.
Serum IgA levels: May be elevated in up to 50% of patients, although this is not diagnostic on its own.
Autoimmune panels: Such as antinuclear antibodies (ANA), antineutrophil cytoplasmic antibodies (ANCA), and complement levels to rule out lupus, ANCA-associated vasculitis, and other autoimmune diseases.
Urine Tests
Urine analysis is essential in the diagnosis of Henoch-Schönlein purpura, particularly to assess kidney involvement:
Dipstick urinalysis may reveal the presence of blood (haematuria) or protein (proteinuria).
Microscopic urinalysis can detect red blood cell casts, which suggest glomerular inflammation.
These findings help stratify the risk of kidney complications and determine the need for long-term monitoring.
Stool Tests and Imaging
In patients with abdominal pain or gastrointestinal bleeding, additional tests may be required:
Stool occult blood test: To check for microscopic bleeding in the digestive tract.
Abdominal ultrasound: Useful in detecting bowel wall thickening, intussusception, or other abdominal complications.
X-ray or CT scan: May be needed in severe cases to identify intestinal obstructions or other structural changes.
Skin or Kidney Biopsy
In atypical or unclear cases—particularly in adults, or when the presentation deviates from the usual pattern. A biopsy may be performed:
Skin biopsy of a purpuric lesion can reveal leukocytoclastic vasculitis with IgA deposits in the small blood vessels when viewed under immunofluorescence.
Kidney biopsy is reserved for patients with significant or worsening kidney symptoms. It typically shows IgA nephropathy or mesangial proliferation in the glomeruli, confirming renal involvement due to HSP.
Diagnosis of Henoch-Schönlein Purpura
Biopsies are not routinely necessary in typical childhood cases but can be instrumental in confirming the diagnosis in adult-onset disease, where conditions like ANCA-associated vasculitis or systemic lupus erythematosus must be ruled out.
Diagnostic Criteria
Several international groups have proposed clinical criteria for the diagnosis of HSP. The most widely used include the EULAR/PRES/PRINTO classification, which requires the presence of palpable purpura (mandatory) with at least one of the following:
Abdominal pain
Joint pain or arthritis
Kidney involvement (haematuria or proteinuria)
Histopathological evidence of IgA deposition
These criteria help standardise diagnosis and ensure consistency in clinical practice and research, particularly in distinguishing HSP from other vasculitides.
Differential Diagnosis
The differential diagnosis for Henoch-Schönlein purpura includes:
Meningococcal septicaemia – a medical emergency presenting with purpura but typically accompanied by high fever, shock, and rapid deterioration.
Idiopathic thrombocytopenic purpura (ITP) – causes bruising and purpura but without the typical joint or abdominal symptoms, and with low platelet counts.
Systemic lupus erythematosus – especially in adolescents and adults, may mimic HSP but with positive autoimmune markers.
Other vasculitides, such as ANCA-associated vasculitis or cryoglobulinaemia, particularly in adult patients.
Diagnosis of Henoch-Schönlein Purpura
In summary, the diagnosis of Henoch-Schönlein purpura is made primarily through a clinical assessment based on a characteristic combination of rash, joint pain, gastrointestinal symptoms, and, in some cases, kidney involvement. Supporting laboratory and imaging tests help confirm the diagnosis, rule out other conditions, and assess for complications. Prompt and accurate diagnosis allows for timely intervention, appropriate monitoring, and improved long-term outcomes, particularly in those at risk of renal disease.