An accurate and timely diagnosis of malaria is critical for initiating appropriate treatment and reducing the risk of severe illness or death.
Since malaria symptoms often look like other illnesses such as flu, typhoid, or dengue, guessing based on symptoms alone can be wrong. That’s why proper testing is key, especially in malaria-prone areas or after travel to those places.
In this section, we’ll look at the main methods used in the Diagnosis of Malaria. These include clinical checks, microscope testing, rapid tests, molecular methods, and how doctors tell it apart from other diseases.
1. Clinical Evaluation in the Diagnosis of Malaria
The first step is a full health check and background history. Doctors usually ask about:
- Travel to malaria zones in the past 12 months
- Risky exposure (such as staying outdoors, no bed nets, visits to rural or forest areas)
- Fever patterns like cycles of chills, sweating, and tiredness
- Any past malaria, especially types that can come back later (P. vivax, P. ovale)
This helps raise suspicion, but by itself, it can’t confirm malaria. That’s why lab testing is always needed.
2. Microscopy: The Gold Standard
Using a microscope to look at stained blood is still the most trusted method for the Diagnosis of Malaria. Two smear types are used:
- Thick smear: Uses more blood, so it’s better at finding even tiny amounts of parasites
- Thin smear: Helps identify the exact type of malaria and shows how much is in the blood
Doctors stain the blood with Giemsa dye, then check under a microscope for parasites in red blood cells.
Pros:
- Shows exact species (P. falciparum, P. vivax, P. ovale, etc.)
- Tells how serious the infection is by measuring parasite levels
- Low cost and widely available
Cons:
- Needs trained staff and good equipment
- Takes time, especially in busy clinics
Even with these limits, microscopy remains the best overall tool when available.
Rapid and Molecular Tools for Malaria Detection
3. Rapid Diagnostic Tests (RDTs)
In places without microscopes, RDTs help confirm malaria quickly. These tests use a drop of blood, usually from a finger-prick, to look for malaria antigens.
They work like pregnancy tests. The most common ones detect:
- HRP2 – only in P. falciparum
- pLDH – found in all malaria types
- Aldolase – seen in multiple types
Benefits:
- Results in 15–30 minutes
- Simple to use with little training
- Great for rural or low-resource areas
Drawbacks:
- May not show which type of malaria is present
- Can’t measure how much parasite is in the blood
- Some tests miss infections, especially if parasite levels are low or if certain antigens are missing
RDTs aren’t as detailed as microscopy but help expand access to testing in high-risk areas.
4. Molecular Tests (PCR and NAATs)
These tests use DNA to find malaria parasites, even when levels are very low. PCR and other NAATs detect parasite DNA in blood samples.
They help with:
- Finding malaria when other tests fail
- Telling apart multiple infections
- Spotting drug-resistant parasites
Pros:
- Very accurate and sensitive
- Good for advanced labs and research
Cons:
- Expensive and slow
- Needs special lab tools and trained staff
- Not suitable for most routine settings
These tests are often used in advanced hospitals, research labs, or in places trying to eliminate malaria completely.
5. Differential Diagnosis
Because malaria looks like many other illnesses, ruling out other diseases is part of the Diagnosis of Malaria.
Other conditions that may be confused with malaria:
- Typhoid
- Dengue
- Leptospirosis
- Flu
- Meningitis
- HIV-related infections
- Viral fevers like Ebola
If malaria tests are negative, doctors need to check for these other causes.
Monitoring and Special Cases in the Diagnosis of Malaria
6. Monitoring and Follow-Up
Even after confirming malaria, more testing may be needed later on.
Doctors use follow-up tests to:
- Check if treatment is working
- Look for drug resistance
- Catch relapses from P. vivax or P. ovale
They may repeat blood smears or RDTs 48–72 hours after treatment starts, especially if the patient isn’t getting better.
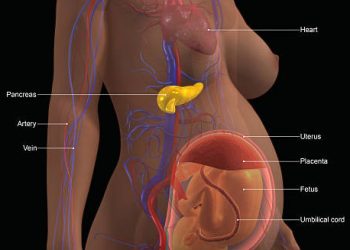
7. Special Considerations in Pregnancy and Children
In pregnant women in malaria areas, the infection may not show symptoms. Routine screening with RDTs or microscopy is important to protect both mother and baby.
Malaria in pregnancy can cause:
- Low birth weight
- Stillbirth
- Placental infection
Children and babies also need close attention. Their symptoms may not follow normal patterns, and they can get worse quickly.
Summary
The Diagnosis of Malaria depends on both signs and lab tests. Microscopy remains the best tool for identifying the type and amount of parasite. But rapid tests make diagnosis possible in places with fewer resources. PCR and similar methods help in special cases.
Early and correct diagnosis is key to stopping malaria, treating it well, and avoiding serious problems or death.