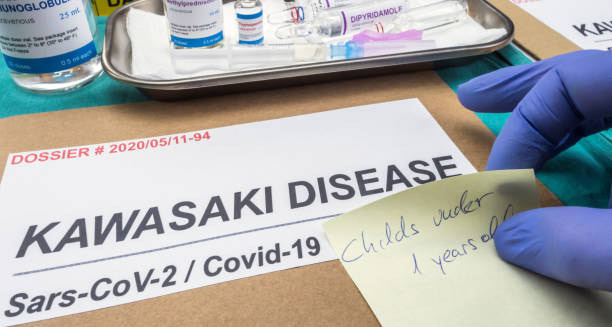
Kawasaki disease is a rare but serious condition that primarily affects children under the age of five.
It causes swelling in blood vessels throughout the body. Doctors call this vasculitis. No one knows the exact cause yet, but the effects can be very serious—especially for the heart. If doctors don’t find and treat Kawasaki disease quickly, it can lead to heart problems. These include inflamed heart muscles, artery swelling, and even heart attacks in young children. Thankfully, with proper treatment, most children recover fully. Still, it remains one of the top causes of acquired heart disease in children living in developed countries.
The illness usually develops in phases. It starts with a lasting fever and includes symptoms like a rash, red eyes, swollen hands and feet, cracked lips, and a red, bumpy tongue. These signs look like many common viral infections, which makes it hard to spot in the early days. That’s why knowing the signs and acting quickly are key to preventing long-term problems.
1. Epidemiology and Demographics
Kawasaki disease mostly affects children between six months and five years old. It is seen more often in boys than girls. Children with East Asian backgrounds—especially from Japan—have the highest rates. However, the disease can appear in all parts of the world, including North America, Europe, and Africa.
In some places, more cases happen during winter and early spring. This seasonal pattern may hint at a trigger. Even so, Kawasaki disease is not contagious. It cannot spread from one child to another.
2. Clinical Presentation and Stages
Kawasaki disease moves through three main stages.
a) Acute Phase (Weeks 1–2):
This stage starts with a high fever over 39°C that lasts more than five days. Other key signs include:
- Red eyes without discharge
- A body-wide rash
- Swollen, red hands and feet
- Cracked lips and a red, bumpy “strawberry” tongue
- Swollen neck glands
The child may seem very cranky and may have belly pain or sore joints.
b) Subacute Phase (Weeks 2–4):
Once the fever goes away, other problems become more visible. These may include:
- Skin peeling on fingers and toes
- Ongoing joint pain
- Vomiting or loose stools
- Continued crankiness
During this time, the risk of heart problems grows. So, close monitoring is very important.
c) Convalescent Phase (Weeks 4–6):
In this stage, most symptoms begin to fade. The child starts to feel better and gains energy. Blood test results slowly return to normal. But the blood vessels may still be healing. That’s why regular check-ups are still needed during this time.
3. Aetiology and Risk Factors
Doctors still don’t know the exact overview of Kawasaki disease and its cause. Most believe the immune system overreacts to an infection. This infection could be from a virus or bacteria. Children with certain genes may respond too strongly, leading to swelling and fever.
There may not be just one germ to blame. Instead, many common germs could be involved in triggering the immune system in certain children.
Risk factors include:
- Age: Most common in kids under five
- Gender: Boys have a higher risk
- Ethnic background: More common in Asian children
- Family history: Siblings may be at slightly higher risk
Even with these factors, not every child exposed to a germ will develop the disease.
4. Prognosis and Outcomes
With fast treatment, most children recover fully in six to eight weeks. The outlook is very good. But if Kawasaki disease is not treated, about one in four children may have heart problems. These may include:
- Swelling in the coronary arteries
- Blood clots
- Heart attacks
- Heart failure
To prevent these, doctors aim to start treatment within the first 10 days of fever. Children who develop heart problems may need care for the rest of their lives.
5. Differential Diagnosis
At first, Kawasaki disease may look like other common illnesses in children. This makes it harder to identify. Other conditions that may look similar include:
- Scarlet fever
- Measles
- Viral rashes
- Stevens-Johnson syndrome
- Toxic shock syndrome
- Juvenile arthritis
What makes Kawasaki disease stand out is a lasting fever plus four or more of the five main signs. These include the red tongue, cracked lips, rash, red eyes, and swollen hands or feet. If a child shows these signs and does not improve with fever medicine or antibiotics, doctors should consider Kawasaki disease right away.
6. Impact on Families and Healthcare Systems
Having a child with Kawasaki disease can be scary and overwhelming. The symptoms appear suddenly and can be severe. Many families need to visit hospitals often. Long-term heart monitoring may also be needed. This puts emotional and financial strain on families.
Because Kawasaki disease is rare, some doctors may not know the latest ways to diagnose or treat it. This can lead to delays in care.
Healthcare systems need to stay informed. It is vital to train healthcare workers, even in places where the disease is not common. Quick access to blood tests, heart scans, and treatments like IVIG (intravenous immunoglobulin) is key to avoiding serious problems.
Final Thoughts on the Overview of Kawasaki Disease
Overview of Kawasaki disease shows us that this illness is a medical emergency. It needs to be caught early and treated right away. Even though the exact cause is still unclear, the way the disease is handled makes a big difference in how children recover.
Most children do very well if they get IVIG therapy early and have their hearts monitored. But a delay in finding and treating it can lead to lasting damage.
By raising awareness, more children can get help in time. Parents, doctors, and caregivers must stay alert to the warning signs—especially a lasting fever in a young child. Quick action can save lives and protect hearts.